We thank Alexandra Spratt and Hunter Kellett at Arnold Ventures for their financial support and intellectual guidance on this project. We thank colleagues at the Center for Economic and Policy Research and Americans for Financial Reform for helpful comments on an earlier draft.
A growing body of research has focused on the social and economic determinants that lead to health inequity among different population groups in the US. People in low-income communities face daily economic challenges, “food deserts,” inadequate housing, and other conditions that undermine their health and well-being.
The structural determinants of health inequity, however, are more hidden from view and have received less attention. By structural determinants we mean health care infrastructure – hospital facilities, technologies, equipment, and other resources – that are critical for health care professionals to deliver quality care to their patients. In this report, we focus on differences in hospitals’ access to capital to finance the construction or modernization of facilities, upgrades to the latest technology, and expansion of services to additional patient populations. Access to funding for capital projects has consequences for the growth of revenue and the financial stability of hospitals and for the quality of patient care.
Central to our argument is that federal government policies and funding formulas played a critical role in fostering these inequalities across health care systems in different communities, especially low-income and rural communities. Our evidence draws on our analysis of federal legislation and IRS tax rulings that have led different types of hospitals to have differential access to public subsidies and capital markets — resources necessary for the construction and upgrading of hospital facilities needed to deliver quality care.
We begin with the 1946 passage of the Hospital Survey and Construction Act known as the “Hill-Burton Act.” The Hill-Burton Act provided extensive public funding for the construction of nonprofit hospitals and was designed to remedy shortages of hospital capacity in poor and rural communities, a goal it largely succeeded in fulfilling. But Hill-Burton also incorporated the racist views and legally and socially enforced segregation of those times into the law, funding separate facilities for Black and white patients. This practice was halted in 1964, but Hill-Burton funding was the largest infusion of public funds to build a nationwide hospital infrastructure in the country’s history. The legacy of racial segregation, inferior hospitals, and worse health outcomes on average for Black patients persists to the present day.
The 1965 Medicare and Medicaid law, which supplanted Hill-Burton, contained a different set of hidden structural inequities. The law provided subsidies to hospitals intended to facilitate their ability to generate internal funds or access financial markets. The Medicare formulas for those subsidies, however, disadvantaged smaller hospitals and those with patient populations insured by Medicaid or not insured at all — especially “safety-net” and rural hospitals. Congressional actions to reduce the federal budget deficit led to an end to those subsidies in the 1990s, and the passage of the 1997 Balanced Budget Act, which substantially cut Medicare and Medicaid reimbursement rates. As a result, hospitals across the country faced financial distress and uncertainty. Even those that had benefited from decades of privileged access to federal resources, such as Academic Medical Centers, faced the prospect of sharp declines in net operating income.
An IRS ruling in 1998 disproportionately helped large nonprofit health care corporations and Academic Medical Centers to access a new source of funding for capital investments. The ruling allowed nonprofit hospitals to create for-profit subsidiaries whose profits were tax-exempt and could be used to subsidize investments in facilities and technology as well as financial activities such as mergers and acquisitions. The legacy of federal funding that disproportionately benefited larger nonprofit systems also positioned them to take advantage of this new ruling. Academic Medical Centers and large nonprofit systems launched partnerships with venture capital (VC) firms, raised funds from capital markets for infrastructure expansion, expanded merger and acquisition (M&A) activity, developed corporate structures, and offered higher compensation packages to CEOs and other executives.
By contrast, rural hospitals and those serving low-income Black, Indigenous, and immigrant communities had aging infrastructure that was most in need of repair and obsolete technologies that needed upgrades; yet they often faced greater challenges in access to capital for investments. This situation was largely unchallenged in the first two decades of the twenty-first century. Passage of the Affordable Care Act and its extension of Medicaid insurance to large swaths of previously uninsured Americans in many states improved the access of millions of people to health care and shored up the finances of hospitals caring for the poorest patients. But Medicaid reimbursements were not sufficiently generous to enable hospitals serving poor urban and rural populations to build up internal resources for financing capital improvement or to improve their access to external funding via financial markets.
The COVID-19 pandemic particularly laid bare the inequities in facilities and technology in rural hospitals, safety-net hospitals, and the largely segregated urban hospitals that treated more Black patients and other people of color compared to white patients. Under the CARES Act of 2020, Congress allocated funds for hospitals to purchase ventilators, oxygen, remote monitoring equipment, personal protective equipment (PPE), and other safety equipment. But surprisingly, the formula for allocating these taxpayer dollars was based on the providers’ share of Medicare payments in a previous year. This disproportionately favored wealthier hospitals — those with higher Medicare reimbursements — over those with lower reimbursements or that were more dependent on Medicaid. This unequal allocation formula exacerbated the gap in the availability of equipment and supplies for rural and safety-net hospitals so vital to saving lives of COVID-19 patients and to providing quality care.
We develop each of these themes in this report.
US policymakers and regulators need to rethink the way that the government finances construction and modernization of health care facilities and technology upgrades. The first step might be a Hill-Burton Act for the twenty-first century that targets new construction, renovation, and modernization of hospitals in communities where it is most needed. Taxing profits above a threshold of for-profit subsidiaries of nonprofit hospitals could subsidize such an initiative.
Since the passage of the Affordable Care Act (Obamacare) in 2010, the US has made significant advances in opening up access to health care for Americans. This is the result of subsidized health insurance premiums for low- to middle-income people and an expansion of Medicaid for low-income people in all but 10 states. Nevertheless, as COVID-19’s tragic effects on Black communities and communities of color showed, America’s health care system continues to provide much better health outcomes on average for white patients than for Black patients, immigrant communities, and for those in low-income urban and rural communities. Stark disparities in health outcomes remain despite improvements in the ability of Americans to access care.
A main approach to understanding differences in health outcomes is to examine the social determinants of health (Pifer 2023) — the social and economic forces that shape people’s lived experience and their health. In contrast, the focus of analysis in this paper might best be referred to as the structural determinants of health, the relationship between the quality of the physical facilities, equipment, and technology, and the safety and quality of patient care. We build on our earlier work in which we examined how health policies, financial deregulation, tax policy, and antitrust policy have interacted to shape the US health system. In particular, hospitals’ unequal access to financial resources has contributed to disparities in the quality of hospitals’ physical infrastructure. Public financing of hospital construction, renovation, and modernization that characterized the two decades following World War II gave way in the 1960s to reliance on financial markets to fund capital projects. Unequal access to financial markets has disadvantaged small hospitals and hospitals that serve poor or rural communities. Academic Medical Centers, in contrast, were able to take advantage of changes in financing that both enriched hospital leadership and provided them with the most modern facilities and cutting edge technologies. In this paper, we examine the impacts of disparities in the quality of hospitals’ physical infrastructure on patient safety and the quality of care.
Investigations into the reasons that health outcomes are so much better on average for Asian1 and white patients than for Black people, Hispanic people, American Indian and Alaska Native people, and other people of color (Hill, Ndugga and Artiga 2024) point to inequities that exist outside the health care system. Social and economic disparities — housing segregation, income inequality, unemployment, homelessness, food deserts, and lack of transportation — negatively affect health outcomes in disadvantaged communities. Black communities and communities of color also experience higher rates of exposure to environmental hazards that affect health, like water pollution, lead poisoning, smog from industrial sites, and emissions from cars. They are also less likely to have access to health care and are likely to utilize health services less frequently.
These long-standing systems of racial bias are difficult to eradicate. Disparities in rates of serious illness and death among different racial groups during the pandemic made it impossible to ignore the serious effects of these inequities on individuals’ health outcomes. “Social determinants of health” have become increasingly prominent in research on health outcomes, with the negative effects of deprivation and marginalization on individuals’ experiences of illness garnering attention. Social inequities that affect the health of women have been singled out as contributing to the stark differences in rates of maternal deaths between Black and white women. According to the Centers for Disease Control, 754 women died of maternal causes in 2019 (Hoyert 2021). Non-Hispanic Black women experienced 44 maternal deaths per 100,000 live births. The rate for non-Hispanic white women was 17.9 and for Hispanic women, it was 12.6. Black women were 2.5 times as likely to die in childbirth or from related causes as white women.
Policymakers have begun to make efforts to address the social determinants of health via interventions designed to help individuals. Screening and referrals by primary care doctors to food assistance, housing programs, nonemergency medical transportation, and community-based care coordination were examined in a simulated study of the cost of these interventions (Basu et al. 2023). This study found that many resources are required to address social needs and that they are largely not included in existing federal programs. Just under half the cost of the interventions was covered by programs like SNAP or housing vouchers, due mainly to capacity constraints in those programs. The Centers for Medicare and Medicaid Services (CMS) is exploring ways to improve health equity and to measure it when evaluating the quality of care provided to Medicare and Medicaid beneficiaries by health providers. However, CMS is limited in what it can do by the fact that it is mainly authorized to reimburse health providers. It recently launched a pilot project to increase payments to primary doctors with the added funds to be used to implement technologies that allow them to better coordinate with social service providers and medical specialists (Olsen 2023; Pifer 2023).
A recent study of racial and ethnic disparities in health outcomes from the Commonwealth Fund finds wide gaps in health outcomes, with outcomes for the Asian population the best of any group and outcomes for the white population better in general than for people of color (Radley et al. 2024). The gap is largest for the Black population. A salient finding is that, nationwide, Black people are about twice as likely to die before the age of 75 from treatable causes compared with white people. The disparities are much lower in some states and generally highest in the 10 states that still have not participated in the Medicaid expansion authorized in the Affordable Care Act (ACA). The Commonwealth Fund study collected data on nine measures of individuals’ health outcomes, five measures of their health access, and 11 measures of their use of health services. It is comprehensive and provides a useful guide to policy measures that can be implemented at the state and local levels to serve underserved communities and reduce racial and ethnic disparities in health outcomes. The policies address some of the most important social determinants of health and seek to improve health outcomes by increasing individuals’ access to and use of a wide array of health services.
This is an important study and the policies it reviews are likely to play a critical role in improving health outcomes. Missing in the Commonwealth Fund study, however, and in nearly all research on disparate health outcomes, is an understanding of how differences in facilities and technology — literally in the quality of the physical structures of hospitals, clinics, and offices where health care is delivered — affect the ability of health professionals to deliver quality care, and in turn, the health outcomes of their patients. That is the focus of this report.
In this report, we highlight a more hidden source of inequality in health care systems. Our focus is on differences in hospitals’ access to the capital needed to finance the construction of new facilities or modernization of buildings, heating and ventilation systems, medical equipment and devices, hardware and software technologies; and expansion of services to additional patient populations. We refer to this through the report as hospitals’ physical infrastructure. Access to funding for capital projects has consequences for the growth of revenue, the financial stability of hospitals (Hudson 2024), and the quality of patient care. The American Hospital Association (AHA) (2021) has noted the aging of hospital infrastructure. It cautioned that the hospitals most in need of infrastructure upgrades may face the greatest challenges in accessing financing for capital investments. In particular, hospitals serving what the AHA refers to as medically underserved populations find it difficult to “update their facilities and remain an access point to care in their communities” (2021:1).
Building on our prior work on the financialization of health care and our analysis of how government funds have been allocated to hospitals and other providers, we argue that unequal access to public funding and financial markets over the last 75 years has led to stark inequalities among health systems in construction and modernization of facilities and in upgrading technology and to a two-tier system of care. Financially stressed hospitals, notably those serving poor urban and rural communities, typically lack modern facilities and up-to-date technology as well as specialists, and may not have access to cutting-edge procedures that can save patients’ lives. They may lack resources even to address patient and worker safety issues. Contrast that with the level of care available at the flagship hospitals of academic medical centers (AMCs), which boast the most modern technology, surgical theaters, and intensive care units as well as a physical setting worthy of a first-class hotel. These disparities contribute to poorer health outcomes observed for Black patients and patients of color relative to white patients (Sarkar 2020; Lasser et al. 2021).
The quality of physical infrastructure affects patient safety (e.g., falls and hip fractures, ulcerated bed sores, hospital-acquired infections) and health outcomes (patients’ perceptions of care, 30-day hospital readmission rates) (Akinleye, McNutt, Lazariu, and McLaughlin 2019). The argument is that a hospital’s financial performance, including operating margins as a proxy for cash flow (Traska 1988), affects its ability to obtain funding for capital investments, hire better-qualified staff, and make costly investments in quality improvement projects (Akinleye, McNutt, Lazariu, and McLaughlin 2019). Hospitals that are profitable are able to repay debt quicker. This enables them to obtain further financing for capital projects at a lower cost than hospitals that are struggling financially. The financing also makes it possible for these hospitals to make upgrades to critical technologies and patient monitoring systems. Improvements in hospital quality and patient safety can be costly to implement and may be limited or foregone by hospitals with poorer financial performance.
An analysis of financial distress in the years 2011 to 2018 found that nearly a quarter of hospitals faced financial distress in each year of the study. For-profit hospitals and those with a higher share of Medicaid revenue were found to have increased odds of financial distress (Enumah and Chang 2021). Three earlier studies of financial distress by the American Hospital Association (AHA), AHA-Urban Institute, and the National Center for Health Services Research carried out in the 1980s found between 20 and 27 percent of hospitals nationally were experiencing financial distress and, further, that the cause of this distress, especially for distressed urban hospitals, arose because they played a large role in caring for uninsured or underinsured patients rather than because of poor or inefficient management (Brecher and Nesbitt 1985). Financial losses lead to less access to capital and higher borrowing costs, constraining investment in critical new technologies (Duffy and Friedman 1993) and in activities to improve quality and safety. Negligent injuries were highest among hospitals in financial distress, many of which served indigent populations (Burstin, Lipsitz, Udvarhelyi, and Brennan 1993). The probability of poor surgical care was higher in safety-net hospitals than in other hospitals (Mouch et al. 2013) and the incidence of immediate breast reconstruction after surgery for breast cancer was lower in hospitals serving disadvantaged patients (Richards 2014). These findings suggest that increased financial pressure leads to declines in investment in infrastructure, including technology, and in measures to improve care. The phasing out of public financing of capital improvements (discussed below in Section 2) has led to a lack of funding for investment in capital improvements or in measures that improve care in safety-net hospitals (Sherlock 1986), which can increase mortality and morbidity rates (Duffy and Friedman 1993).
Tragically, the COVID-19 pandemic provided a context in which researchers could analyze the factors that contributed to deaths from the disease. Black patients were more likely to die than white patients, but was the difference related to race, or were there other factors that determined patient outcomes? The earliest studies were based on relatively small samples of patients treated by single health systems. These studies found that differences in demographic factors (age, gender) and comorbidities (obesity, diabetes, other chronic conditions) explained the observed differences in mortality rates. Asch, Islam, and colleagues (2021) used the large population of Medicare beneficiaries hospitalized with COVID-19 to carry out a more comprehensive analysis of the factors contributing to the higher mortality of Black patients compared to white patients. They were interested in understanding whether the hospitals where patients were treated also impacted death rates for Black and white patients. To answer this question, the researchers analyzed a cohort of 44,212 Medicare Advantage enrollees with a diagnosis of COVID-19 who were admitted to 1188 acute care hospitals between January 1, 2020, and September 21, 2020, overcoming the sample size and single health system limitations of other studies. This sample was not only much larger, but it was also likely to be more heterogeneous than those in studies that found no role for race in explaining the observed disparity in mortality between Black and white COVID-19 patients.
The researchers first carried out the analysis of this disparity by examining the association between mortality and a wide range of personal characteristics and comorbidities. Mortality is defined in this study as death or discharge to hospice within 30 days of admission to the hospital. They adjusted the mortality rates of Black and white patients for age, sex, income level, zip code, 23 specific comorbidities, and admission to hospital from a nursing facility. They also adjusted for the number of days between January 1, 2020, and the date of admission to account for likely improvements in patient outcomes as hospitals gained experience, for census regions to account for geographic variation in care, and for COVID-19 surges over time.
To examine the association with the hospital itself, the researchers adjusted for the specific hospitals to which patients were admitted. Finally, they used simulation modeling to estimate the mortality among Black patients had they instead been admitted to the hospitals where white patients were admitted. But Black patients still had greater 30-day odds of inpatient mortality or discharge to hospice compared with white patients. Black patients had an adjusted risk of mortality that was greater than white patients, 12.32 percent compared with 11.27 percent. The difference is statistically significant. However, after further adjustment for hospital-level fixed effects (basic characteristics such as number of beds, ownership status, and others) of the admitting hospital, mortality outcomes for Black patients were not statistically different than for white patients. The hospital at which a patient was treated made a difference in their chances of dying from COVID-19.
Black patients were disproportionately treated in hospitals with higher proportions of Black patients. In the simulation exercise, the researchers found that had the Black patients been assigned to the same hospitals as white patients and in the same proportions, their risk of mortality from COVID-19 would have been significantly reduced.
The researchers conclude that differences in the mortality outcomes of Black and white patients “were partly explained by adjustment for social, demographic, and clinical factors.” But “even after adjustment for those factors, racial differences in the mortality of patients” remained. “Those differences are almost entirely explained by the hospitals to which Black and White patients were admitted.” The researchers point to “uneven resourcing and quality of hospitals that provide care to a disproportionate number of Black patients” as a key source of higher death rates for Black COVID-19 patients (Asch and Islam et al. 2021: online page 9/11).
A recent study of a large-scale intervention by the philanthropy Duke Endowment that upgraded the physical infrastructure of hospitals in North Carolina in the first half of the twentieth century demonstrates the positive effects of such investments on health outcomes. The researchers examined the effects of the modernization of hospitals’ physical facilities on the death rates of Black and white infants. They found that the upgrading of facilities made possible by Duke Endowment’s financing of hospital modernization led to a 7.5 percent reduction in the infant mortality rate — a drop of 13.6 percent for Black infants and 4.7 percent for white infants. The effects of these improvements in hospitals’ physical infrastructure led to better quality patient care that persisted for decades. They attributed this to complementarity between the quality of hospital infrastructure, attraction of higher skilled physicians, and adoption of health care innovations (Hollingsworth, Karbownik, Thomasson and Wray (2024).
Studies of the role of hospital quality rarely examine the quality of the hospital’s built environment. The exception is research on rural hospitals. Here it is more obvious that disparities in investments in renovation and modernization have left the facilities in poor physical condition and unable to meet high standards of care. Operating rooms may be too small to utilize the latest technology to perform particular surgeries for example, and the hospitals are generally less able to provide the highest quality care. A great many rural hospitals were built with public funds appropriated in the Hill-Burton Act, discussed below. This source of funding ended in 1997. Hospitals built with these funds are anywhere from 35 to 60 years old or older and face the challenge of upgrading their facilities as they receive reduced payments for their services from public and private insurance payers. The aging infrastructure of rural hospitals is a major worry for the communities they serve. Most rural hospitals operate at very low margins and may be unattractive to private lenders. They find it difficult to “qualify for loans or other types of financing to upgrade their facilities to meet the ever-changing standards of medical care” (Hawryluk 2024).
Disparities in access to funding for hospitals’ investment in facilities lie in laws and regulations dating back to at least the end of WWII and their evolution in the following decades — health policies, financial deregulation, tax rules, and the reversal in anti-trust guidelines. The legal framework is a patchwork of different laws and regulations with different incentive structures that were enacted without reference to one another (Appendix Table 1). The most important laws and regulations include health care policy (1946 Hill-Burton Act, 1965 Medicare and Medicaid Act, 2010 Affordable Care Act); tax policy (1960 Real Estate Investment Trust (REIT) Act, 1969 IRS ruling that expanded what counts as charitable purposes so that a hospital’s charity care did not need to include care of the indigent and a 1998 IRS ruling that allowed nonprofit hospitals to set up tax-exempt for-profit subsidiaries); anti-trust policy (including the reversal in antitrust guidelines during the Reagan administration that promoted consolidation); and financial deregulation (including changes in pension law) that opened large pools of capital for investment by Wall Street firms.
As we discuss in Section 2, the Hill-Burton Act of 1946 provided public funds for the construction of nonprofit hospitals, nursing homes, and clinics. The Act greatly expanded the available number of beds and increased access to such facilities by building many of them in counties that in 1945 had no hospital. The Hill-Burton Act is a story of successful investment in medical infrastructure, but it is also a tale of perpetuating segregation. It officially institutionalized structural racism by financing “separate but equal facilities” that often were not equal and spurred unequal access to funds for the construction and modernization of hospitals and facilities that served Black communities.
Public financing of hospital construction was phased out over a period of nearly three decades after the legislation authorizing Medicare and Medicaid was implemented. Medicare, as we discuss in Section 3, subsidized the costs of new construction as well as modernization of existing facilities. It provided hospitals — including, for the first time, for-profit and nonprofit hospitals — a subsidy that covered capital costs such as interest on debt, including debt incurred in acquiring other hospitals, as well as depreciation. It also included an add-on of 2 percent of these costs for the construction of new facilities. Unlike Hill-Burton funding, the subsidies did not cover the actual cost of the capital investment. What it covered was the cost of capital, mainly interest on borrowed funds and depreciation. Nonprofits were now competing directly with for-profit hospitals in financial markets for funding for the construction and modernization of facilities. Funding sources for capital projects of nonprofit hospitals, including charitable grants from wealthy donors and government grants and appropriations, fell steeply from 44 percent in 1968 to just 16 percent in 1981 of investments in hospital infrastructure. This decrease meant that nonprofit hospitals increasingly relied on borrowing in financial markets to raise funds for investment in facilities and technology. Nonprofit hospitals were held to the same underwriting standards as for-profit hospitals when borrowing in financial markets (Heshmat 1992). This disadvantaged small hospitals and hospitals serving uninsured and underinsured patients in poor urban and rural communities that could not meet the financial performance requirements to qualify for these loans.
For-profit hospitals also received a premium so that they could pay dividends to their shareholders. (Grogan 2023). These subsidies allowed for-profit hospitals, with their prior relationships with financial market actors, to obtain nearly risk-free loans for the construction of new facilities and the acquisition of existing health organizations as they built large chains (Fox and Schaffer 1991). The change in antitrust guidelines allowed these hospital mergers to proceed unchallenged.
Changes in rules on the use of tax-free bonds by nonprofit hospitals opened up their access to financial markets for construction and modernization. But the playing field wasn’t level as the legacy of structural racism denied access to financial markets for some hospitals. The Medicare subsidies provided assurances that loans could be repaid. But lenders applied the usual underwriting criteria nevertheless, and favored hospitals in more affluent neighborhoods, those with a payer mix that included commercial health insurers as well as Medicare, and those that typically served mostly white patients. Black, Brown, and poor white communities in urban and rural areas were often unable to access funds for the construction of new facilities or for upgrading existing buildings and technology (Grogan 2023).
The 1998 change in IRS guidelines allowed nonprofit hospitals to own, tax-free, for-profit subsidiaries. We examine the effects of this on disparities in physical infrastructure and patient outcomes in Section 4. The tax guidance set the stage for an alliance between academic medical centers (AMCs) or other large nonprofit hospitals with a capacity for medical research on the one hand and venture capital firms that sponsored start-ups on the other. This alliance of health care and Silicon Valley was established to create patentable medical products and processes. While initially a lifeline to cash-strapped hospitals hurt by Congressional budget balancing cuts and a shift in Medicare spending from AMCs to hospitals treating a disproportionate share of poor patients, this alliance with venture capital soon turned into a windfall. It enriched some of the most well-endowed hospitals in the US, exacerbating inequalities in facilities and their ability to treat patients. In principle, these nonprofit hospitals could afford to offer reduced cost or free care to poor patients which would mitigate the effects of disparities in the quality of facilities. But in fact many spent less on the care of indigent patients than they received in tax breaks. Some even refused to accept transfers of patients during the COVID-19 pandemic from hospitals that lacked life-saving equipment even when they had empty beds (Schorsch 2020).
The challenges facing rural hospitals with aging facilities and technology are discussed in Section 5. These hospitals play a major role in securing the health of rural populations and often are major economic anchor institutions providing stable employment to residents of their community. Maintaining these facilities, and renovating them to meet changes in patient preferences and how hospitals best treat patients, is key to the vitality of rural communities. But rural hospitals face major challenges to their ability to upgrade facilities and technology, staffing, financing, low patient volumes, and aging infrastructure. Their small size, thin margins, and heavy reliance on Medicaid as payers puts many of these hospitals at a disadvantage. Keeping up with advances in physical infrastructure including technology and equipment requires high operating margins. High margins facilitate the accumulation of internal reserves for construction as well as the ability to borrow in financial markets. Hospitals that can invest in facilities and technology are able to attract patients and doctors. They are on an upward trajectory. Less fortunate hospitals that lack access to funds for construction, renovation, and modernization will lose patients and have difficulty recruiting and retaining physicians. They will find themselves on a downward trajectory and, if something doesn’t intervene, will continue to wither and fail. In light of the important role that they play, can they be restored to health?
The disparities in access to funding came to a head during the COVID-19 pandemic, as we discuss in Section 6. The all-important first tranche of funding from the CARES Act early in the pandemic was distributed with no strings attached to health organizations based on the share of Medicare (but not Medicaid or charity care) patients the provider organization had treated in the preceding year. A nontrivial part of the explanation of higher COVID-19 death rates in Black communities compared to white communities rests with the hospitals in which Black patients were treated.
The Conclusion looks at the urgent need to address and remedy disparities in physical infrastructure and technology among hospitals. Current methods of funding hospitals’ capital investments widen the inequities in hospital infrastructure and the quality of patient care.
The Hospital Survey and Construction Act of 1946 — which came to be known as the “Hill-Burton Act” — is one of the largest federal investments in hospitals and other medical facilities in United States history. Following World War II, President Harry Truman presented five goals to improve the health of Americans. The least controversial of these was his call to construct hospitals and clinics to serve a growing population (Schumann 2016). Congress responded with the Hill-Burton Act,
The main goal of Hill-Burton was to increase the number of hospital beds available across the country from the insufficient level of 3.2 beds per 1,000 civilian population in 1945 to 4.5 beds per 1,000 (Chung, Gaynor, and Richards-Shubik 2016). Demand for hospital beds far outran supply following the end of World War II. The Hill-Burton Act provided $75 million a year for five years in grants to states for hospital construction beginning in 1947. In 2023 dollars, this is about $1.06 billion. The amount was raised to $150 million in 1949, which is $2.1 billion in 2023 dollars. Hill-Burton also provided substantial funding so that states could conduct surveys to determine how to allocate construction loans and grants. In total, between 1946 and 1971, a total of $3.7 billion in federal funding and $9.1 billion in matching funds from state and local governments was allocated (Clark et al. 1980). In the decades that followed 1946, general hospitals, mental hospitals, tuberculosis/chronic disease hospitals, public health centers, nursing homes, diagnostic and treatment centers, and rehabilitation centers were built all around the US.
Over that period, there were a total of 10,490 projects funded by the Hill-Burton program. Of these, there were 5,567 projects focused on short-term general hospitals. The program was designed to remedy perceived shortages of hospital capacity in poor and rural communities. These factors played an important role in how the funds were distributed and in the increase in the supply of hospital beds per 1,000 population. Geographic areas with a low supply of beds per 1,000 in 1947 mostly caught up with areas that had more hospital capacity by 1971. The South added more beds per 1,000 than the Northeast. Rural areas had the largest increases. Across counties, the variation in beds per 1,000 narrowed considerably; it fell by more than half between 1948 and 1975. Substantial progress was made in expanding the number of hospital beds in poor and rural areas and making access to hospitals more equal throughout the US. Hospital admissions increased in line with the increase in hospital capacity. These results suggest that the Hill-Burton program had a substantial net positive on hospital capacity and the distribution of hospital beds in the US as well as on access and utilization (Chung, Gaynor and Shubik 2016).
Until the passage of the Hill-Burton Act, there were no hospitals in many parts of the rural South. The hospitals were almost entirely racially segregated into different facilities, and there was a lack of investment in the Black facilities (Beardsley 1987). The small number that did exist were mostly small, poorly equipped private institutions concentrated in urban areas, and largely closed to Black patients (Thomas 2008). The alternative to the white facilities were the small hospitals and nurses’ training schools run by Black physicians. Before the 1930s these were often the only places where Black people could go for medical attention (Beardsley 1987, 37). In 1940 in 16 southern states, 9.7 million African Americans were served by 79 black hospitals, most of which were unaccredited, underequipped, and struggling to keep their doors open (Thomas 2006). There was also a lack of personnel, lack of training for Black medical professionals, and discrimination in their hiring.
The idea of Hill-Burton was to provide funds to communities in need so long as they could demonstrate that a hospital or other medical facility would be sustainable based on the communities’ population and per capita income. Forty percent of counties that did not have a hospital in 1945 saw construction break ground. Many of these new hospitals and other medical facilities were in the South and more grant money went to low-income states (Lave and Lave 1974, 17).
The Hill-Burton Act is a story of successful investment in medical infrastructure, but it is also a tale of perpetuating racial segregation. The legislation’s nondiscrimination clause required that hospitals built with federal Hill-Burton money admit all people regardless of “race, creed, or color.” However, there was a catch. States that already had “separate but equal facilities … for separate population groups” could ignore the nondiscrimination provision so long as they supplied Black people with enough facilities and services “of like quality” to meet the assessed need (Beardsley 1987, 178; Thomas 2006, 839). The Act institutionalized existing patterns of discrimination and enshrined “separate but equal” into the US hospital system. By legally sanctioning hospitals to continue existing patterns of discrimination, the Hill-Burton Act reinforced structural racism and appeased pro-segregation Southern lawmakers who demanded the independence of state legislatures (Largent 2018).
The nature of segregation in hospitals and other facilities went from “spatial isolation in completely separate buildings to the partitioning of racial groups within shared structures via separate entrances, floors, wards, etc.” (Thomas 2006). The federal Public Health Service (PHS), which today is part of the Department of Health and Human Services, accepted statewide hospital plans that included segregated institutions as long as the state health planning agency considered these facilities adequate for the population served. As Edward Beardsley wrote in his 1987 book, Hill-Burton “left it to Southern states (and the surgeon general as final arbiter) to decide how much blacks needed” (178).
In Congressional debates at the time, some Senators, Northerners in particular, spoke out against discrimination and argued that no federal funds should go to hospitals that practiced segregation. Southern Democratic segregationists argued for states’ rights and letting hospitals set their own policies. The compromise language prohibited outright discrimination by race but permitted separate but equal funding for hospital construction (Harvard University 2020). The provision was the only one in federal legislation of the 20th century that explicitly permitted the use of federal funds to provide racially exclusionary services (Largent 2018). By 1975, a third of all hospitals in the US had been constructed using Hill-Burton funding.
Direct federal funding of hospital and health facilities construction ended in 1997. By that time, the Hill-Burton Act had partly financed about 6,800 facilities in 4,000 communities, including hospitals, clinics, rehabilitation centers, nursing homes, and long-term care facilities (Clark et al.1980). By this point, Hill-Burton was folded into bigger legislation called the Public Health Services Act. Data from 10 years after the Hill-Burton Act’s passage showed that fully integrated hospitals where Black people were admitted to any available hospital bed were rare (Cornely 1956).
For most of the hospitals that received Hill-Burton funds, the separate Black wings that were constructed had poorer nurse staffing, fewer visiting hours for families, and the facilities were outdated and crowded. Black physicians were barred from treating patients throughout the wards. Through the 1950s, most Hill-Burton hospitals, especially in the South, remained closed to Black medical interns, refused to employ Black residents, and generally denied Black physicians the opportunity to treat Black patients (Beardsley 1987).
Black physicians were a well organized, elemental group in the movement to end hospital segregation (Beardsley 1987). There was a wide range of opinions within the Black community towards how the hospital system should progress. Black physicians in the National Medical Association promoted federal enforcement of racial parity in health care and were staunchly against the original version of Hill-Burton, whereas other groups of Black physicians and civil rights leaders were in favor of increased funding even if it came with strings attached (Meltsner 1966). The American Medical Association, one of the largest associations of physicians, was silent on the development of the Civil Rights Act and put off requests to amend Hill-Burton’s “separate but equal” provision.
Litigation over discrimination in the medical facilities was limited and received little public attention for about two decades following the 1946 Hill-Burton passage. The National Association for the Advancement of Colored People (NAACP) led several lawsuits to eliminate discrimination in hospitals.
Finally, in the 1963 case Simkins v. Moses H. Cone Memorial Hospital, the NAACP succeeded in having a US Court of Appeals overturn the “separate but equal” part of Hill-Burton. At the time there were only nine hospitals that served Black people in all of North Carolina. The Moses H. Cone Memorial Hospital and the L. Richardson Memorial Hospital in Greensboro had received funds from Hill-Burton even though they were both closed to Black patients because the state regulatory body had approved it.
The critical argument of the case was not centered around the differences in the facilities that treated Black and white patients, even though this was certainly occurring. Instead, George Simkins, along with other Black doctors in the state who were supported by the NAACP, made the argument that these private institutions were engaged in “state action” because they received Hill-Burton funds, and thus were subject to the US Constitution’s prohibition of racial discrimination under the Fifth and Fourteenth Amendments. The court agreed and ruled that the Public Health Service Regulations set in motion by Hill-Burton of providing separate but equal services in Hill-Burton hospitals were unconstitutional. (Thomas 2006).
Legal precedent for hospital integration continued to build on a national level. A year later in 1964, the Civil Rights Act was passed. All facilities receiving federal funds like Hill-Burton were required to abide by Title VI, which said that “no person in the United States shall, on the ground of race, color, or national origin, be excluded from participation in, be denied the benefits of, or be subjected to discrimination under any program or activity receiving federal financial assistance” (US Department of Justice). This legislation was a vital step towards preventing federal funds from going to public and private institutions open to the public that discriminated against Black Americans (US Commission on Civil Rights). Yet, the task of desegregating hospitals was enormous. Survey data showed that in early 1966 only 42 percent of hospital beds in the US were in hospitals that were compliant with Title VI.
In 1966, after being signed into law by President Johnson the year prior, the Medicare program went into effect and became a critical tool in the push toward stopping hospital facility segregation. Suddenly, the federal government would pay millions for the care of elderly and disabled people. Strategically, the Department of Health, Education, and Welfare was directed by President Johnson’s Administration to require immediate integration if hospitals wanted to receive their Medicare certification and open the spigot of Medicare money.
Many Southern hospitals threatened to forego Medicare funding and deny care to seniors. A pressure campaign by members of President Lyndon Johnson’s administration averted that disaster, and hospitals all over the country, including in the South, desegregated (Harvard University Center for the History of Medicine at Countway Library 2020; Reynolds 2004). By July 1966, 2,000 hospitals integrated (Ross 2015). If not for the passage of Medicare and its strong enforcement by Johnson’s administration, lawyers and groups like the NAACP would have had to take each individual health care facility to court with resources they didn’t have (Smith 2016).
There are lasting impacts of Hill-Burton: Black patients are overwhelmingly treated in a small number of hospitals that mainly treat Black patients. A Harvard University study of the 4,455 medical and surgical hospitals in the US that treated Medicare patients in 2004 found that just 222 of these hospitals treated a disproportionate number of Black Medicare beneficiaries. These 222 hospitals, just five percent of hospitals with the highest volume of Black patients, cared for nearly 44 percent of all elderly Black Medicare patients. The top five percent with the highest share of Black patients cared for approximately 23 percent of Black seniors. In contrast, the top five percent with the highest volume of white patients provided care for 23 percent of white seniors, while the five percent with the highest share of white patients cared for just 0.7 percent of white Medicare beneficiaries (Jha, Orav, Li and Epstein (2007).
The segregation of elderly Black patients had deadly effects during the COVID-19 pandemic. Black COVID-19 patients were substantially more likely than their white counterparts to die from the disease. The large-scale study of COVID-19 deaths described earlier in Section 1.2 (Asch and Islam 2021) found that Black patients were disproportionately treated in hospitals with higher proportions of Black patients (See Figure below). In the simulation exercise they conducted, the researchers found that had the Black patients been assigned to the same hospitals as white patients and in the same proportions, their risk of mortality from COVID-19 would have been significantly reduced. They point to differences in the quality of hospitals as a key source of higher death rates for Black COVID-19 patients.
The 1965 amendments to the Social Security Act established the Medicare and Medicaid programs, currently overseen by the Centers for Medicare and Medicaid Services (CMS). This legislation had a profound effect on the US health system. In addition to its familiar role of providing federal health insurance for people over age 65 and certain people with disabilities, Medicare also provided payments to hospitals to cover their capital costs. Medicare displaced Hill-Burton, which was gradually phased out, as the major source of public funding for modernization and new construction of hospitals and other health facilities. Direct funding of nonprofit hospital construction under Hill-Burton ended in 1997.
Medicare legislation had a serious impact on the delivery of health care by hospitals in two ways. First, it subsidized capital costs for both for-profit and nonprofit hospitals, the first time that for-profit health organizations received public funds. Medicare provided payments to hospitals for existing capital-related costs such as interest on debt, including debt incurred in acquiring other hospitals, insurance, and depreciation. For a time, Medicare also provided a 2 percent add-on for capital improvements. In effect, Medicare provided a subsidy to hospitals for construction of facilities by covering associated capital costs. Importantly, however, it did not cover the actual costs of construction and modernization. This was a new situation for nonprofit hospitals. Much of the costs for building and modernizing facilities had been covered under Hill-Burton, especially in the case of hospitals serving poor or rural communities. As had always been true of for-profit hospitals, nonprofit hospitals would now have to seek all of that funding in financial markets (Grogan 2023; Mayes and Berenson 2006 ).
Second, Medicare greatly increased hospital admissions by increasing access to health care among the nation’s elderly. It reimbursed hospitals for the care of beneficiaries by reimbursing the fees charged for medical care of hospitalized seniors on a cost-plus basis. This substantially reduced financial pressures on hospitals. In addition, Medicaid reduced the amount of uncompensated or charity care provided by hospitals, thus improving their bottom lines (Mayes and Berenson 2006).
Medicare’s payments to hospitals to cover the costs associated with investments in capital (interest on debt incurred in construction or acquisition of facilities as well as, depreciation, and insurance) acted as a subsidy to hospitals. These payments were larger for more successful and better-endowed hospitals as these were more likely to have engaged in expansion via new construction and acquisition and thus to have higher interest payments and depreciation. The Medicare subsidy made the issuance of tax-free municipal bonds by larger nonprofits attractive to lenders. These hospitals were able to raise funds for capital investments by issuing municipal bonds. Subsidies to smaller and/or poorer hospitals were less generous and, in the case of hospitals that were struggling financially, these payments were often used to meet operating expenses. As a result, access to financing for capital expenditures via financial markets was very uneven. It reinforced disparities among nonprofit hospitals in the quality of their physical plant. Issuing tax-free municipal bonds to finance the construction of facilities was daunting for smaller hospitals and those that served a high number of poor, uninsured, or underinsured patients. These hospitals were not seen as good credit risks, and their difficulties obtaining funding for capital investments widened the gaps among hospitals in the quality of facilities.2
But municipal bonds were not a panacea. Wall Street banks lost no time marketing risky financial instruments to hospitals to reduce their interest payments on the bonds. Rising interest rates in the 1970s and early 1980s were a challenge for hospitals. The main risk in the two and a half decades preceding the bursting of the housing bubble and the financial crisis of 2008–2009 was that interest rates would increase. Lenders demanded variable rate bonds when lending long-term, and Wall Street banks peddled derivatives to nonprofit hospitals without explaining the downside risks or offering a hedge against a decline in interest rates.
Nonprofit hospitals made use of two main financial instruments to manage the risk that interest rates might rise: interest rate swaps and auction rate securities. Interest rate swaps changed the type of interest rate they had to pay from a variable rate to a fixed rate. Many nonprofit hospitals used such swaps to exchange their variable rate bonds for fixed rates paid to a bank. If interest rates were to rise above the fixed rate, the bank would be the loser. The risk has been shifted to the bank. But if interest rates fell below the fixed rate, the hospital would be the losing party. The risks to the hospital from engaging in the swap were downplayed by banks. By 2005, swaps were used by 70 percent of large hospitals (Cleverly and Baserman 2005:364) convinced by Wall Street banks that interest rates were low and could only rise. They were lured by the false pretense that interest rates could not get any lower (Dugan 2010:1).
Unfortunately for the nonprofit hospitals, interest rates could, and would, fall. Banks were on the hook for major losses. Facing the prospect of drawn-out, unnecessarily inflated interest rate payments, hospitals were forced to pay millions of dollars to terminate these unsuccessful bets on the direction of interest rates (Dugan 2010; McDaniels 2013). Even if hospitals escaped having to pay staggering fees to cancel their swaps, many still suffered from having to allocate a sizable portion of their cash reserves to collateral for the swaps (Walker and The Baltimore Sun 2013; Evans 2010). After this experience, many hospital systems retreated from the use of interest-rate securities.
Auction rate securities (ARSs) were another financial instrument used by hospitals to manage interest on their long-term debt. ARSs became widely used among hospitals; by 2007, the market for ARSs was estimated to be as high as $330 billion. They were particularly attractive for hospitals because they allowed for the financing of long-term debt with short-term interest rates, and in many instances, broker-dealers touted ARSs as being nearly risk-free and highly liquid. In the end, the opposite proved to be true. ARS’ uniqueness lay in regular intervals whereby hospitals’ interest rates would be reset by Dutch auction, essentially creating floating rates. (D’Silva, Gregg, and Marshall 2008). Investment banks promised to be a buyer of last resort, preventing a failure in the market.
ARS bonds earned banks more than $1 billion in fees at the initial sale plus annual payments for handling the auctions of a quarter percentage point, or about $650 million a year (Stewart and Smith 2012). Later, Citigroup and UBS were investigated for misleading nonprofit hospitals. ARS made up a significant portion of many hospitals’ long-term debt (Stewart and Smith 2012).
For a period of time, ARSs functioned well for hospitals. But this ended in 2008 with the downgrading of financial institutions amid the housing and financial crisis. A loss of faith in the willingness of financial institutions to back the auctions led to high failure rates of the auctions. The investment banks that promised to be lenders of last resort backed out, citing strain from the ongoing financial crisis and mortgage lending defaults (Greene 2008). The failure of the ARS market had a drastic and scarring impact on hospitals from coast to coast, forcing hospitals to backtrack on intentions to build new facilities (Dugan 2010).
More recently, nonprofit hospital systems avoided derivatives, preferring to refinance municipal bonds if interest rates fall. But this strategy was closed off by the 2017 Trump Administration’s Tax Cuts and Jobs Act (TCJA) which ruled out advance refunding of municipal bonds. Hospitals were no longer able to take advantage of a fall in interest rates (Stewart and Owhoso 2004; Rose 2012; Bannow 2019; Franklin 2020).
Tax-free municipal bonds remain an important source of funds for construction, expansion, renovation, and modernization of hospital facilities. But hospitals are more cautious in managing their debt.
While raising investment funds in capital markets proved challenging for nonprofit hospitals, the cost-plus payment arrangements by Medicare and Medicaid for reimbursing the costs of caring for eligible seniors was a boon to all hospitals. It insulated them from the vagaries of demand for hospital services and provided a buffer of reliable payments for care of a significant share of their patient populations.
But cost-plus payments also meant a lack of constraints on pricing for doctor and hospital services. Prices for procedures varied widely and health care costs trended up. This arrangement began to come under pressure in the late 1970s and early 1980s as the inflation rate began rising more steeply and medical fees increased rapidly. This began to threaten the solvency of the Medicare program. That caught the attention of Congressional policymakers and focused attention on health care prices. A number of modest measures intended to slow the rate of health care inflation were adopted but had little effect (Mayes and Berenson 2006). Bolder action would be needed to secure the solvency of Medicare.3
In 1983, Congress made drastic changes in the way that Medicare reimbursed hospitals. Instead of reimbursing hospitals on a cost-plus basis for every service the patient receives (fee-for-service payments that covered separate charges for doctors’ services, lab tests, procedures, and hospital stays), Medicare instituted a “prospective payment” system. Under this system, hospitals received a predetermined payment for treating Medicare patients depending on their particular diagnosis, referred to as diagnostically related groups or DRGs (Mayes and Berenson 2006). This change in payments to hospitals did not apply to Medicaid, which continued to use either a fee-for-service payment model or, more commonly, a Managed Care Plan (capitated payments made on a per-enrolled person in the plan) to pay for Medicaid benefits (Scott 1984).
The introduction of Medicare Severity Diagnostic Related Groups (MS-DRGs) as the basis for reimbursements for procedures and stays at acute care hospitals marked Medicare’s transition from a cost-plus reimbursement model to a prospective payments model. In this payment model, Medicare prospectively sets the rates hospitals receive for most services. If a patient can be treated at a lower cost, as a result of fewer tests or a shorter hospital stay, for example, the hospital keeps the difference. If the cost of treating a patient exceeds the Medicare payment, the hospital absorbs the extra costs (Mayes and Berenson 2006).
Medicare provides a clear description of prospective payments to hospitals for operating costs and capital costs in its online publication MLN Educational Tool/Medicare Payment Plans (2024). In-patient hospital discharges are examined and assigned to the appropriate MS-DRG category. This takes into account the severity of the patient’s illness, complexity of service, and consumption of hospital resources as well as diagnoses (up to 25), procedures performed (up to 25), sex, age, and discharge status.
Hospitals receive operating and cost-of-capital payments based on patients’ MS-DRG status. Operating costs cover labor and supplies, while capital-related costs cover depreciation, interest, rent, and property-related insurance and taxes. Payment rates are adjusted annually to reflect (1) any changes in treatment costs compared to average Medicare treatment costs and (2) any changes in local market conditions compared to national conditions (e.g., wage rates).
The changes in how hospitals are paid put a premium on hospitals’ ability to control costs related to purchasing, inventory, staffing, and scheduling. Hospital administrators also encouraged doctors to reduce the length of patient stays and move patient care outside of hospitals to facilities (out-patient surgery center, skilled nursing facilities) that had lower costs. At the time prospective payments were first introduced, outpatient care received more generous Medicare reimbursements (Mayes and Berenson 2006). Medicare responded to pressures to curb the growth of payments for MS-DRGs by ratcheting down the annual increases. By 1989, the growth in Medicare expenditures had fallen to just 1 percent a year. This improvement for Medicare translated into a substantial decline in hospital Medicare operating margins and, for some hospitals, including academic medical centers, overall operating margins declined (Henderson 2015).
Leaving financing of construction, modernization, and expansion to the tender mercies of financial markets has led to unequal funding for capital investments and unequal quality of hospitals’ physical plants. In both the original Medicare cost-plus reimbursement model and in the MS-DRG model, bigger and better-endowed hospital systems receive larger payments than smaller or poorer hospitals by virtue of having higher depreciation, interest, and other property-related payments. These payments act as subsidies to the hospitals that facilitate the issuance of tax-free municipal bonds and other borrowing in capital markets, disadvantaging smaller and poorer hospitals. The result is a two-tier hospital system with poor and/or uninsured or underinsured patients more likely to be treated in hospitals with an inferior physical plant, outdated technology, and fewer specialists. A lack of resources and physical capacity may lead these hospitals to triage patients out of necessity, treating those more likely to recover and paying less attention to those with more acute health problems.
For-profit hospitals did not begin to be a serious presence in health care until 1965 and the establishment of Medicare and Medicaid. We noted briefly that Medicare provided reimbursements to for-profit as well as nonprofit hospitals and health systems. Unlike philanthropic donations or Hill-Burton payments for capital investments, Medicare payments subsidized the upgrading of facilities by covering costs associated with capital investments. Funds to cover the actual cost of construction and modernization of hospital facilities would have to be borrowed from financial markets.
Medicare reimbursements to for-profit providers were more generous than reimbursements to nonprofit or public (government-owned) hospitals. Medicare paid for-profits a premium based on the logic that they needed additional capital payments to provide a return on shareholders’ investments. This “virtually guaranteed for-profit facilities a ‘risk-free’ investment return” (Jeurissen et al. 2021:71). For-profit hospitals also benefited from government reimbursements for their interest payments on debt from buying up additional hospitals, while tax laws permitted them to claim accelerated depreciation. With higher relative government subsidies, the for-profit chains grew at a faster rate than nonprofit hospitals, and their share of hospital beds doubled to 9 percent by the early 1980s (Jeurissen et al. 2021: 71).
This method of subsidizing hospitals had three negative outcomes that continue to plague the US health care system to this day (Grogan 2023).
The IRS was complicit in the development of a two-tier health system, having issued the regulation in 1969 that changed the definition of charity as discussed above (IRS 1969). No longer did nonprofit hospitals have to treat indigent patients to qualify for nonprofit tax status with its exemption from most income, property, and sales taxes. Health education for local communities, financial support for the education and training of medical residents, and the shortfall in Medicaid payments for procedures compared to Medicare payments, among other activities, now counted as charitable contributions.
Over the past two decades, Academic Medical Centers (AMCs) went from being on the verge of financial crisis to being the most financially stable type of nonprofit hospital. This transformation is in large part due to shifts in IRS guidelines which opened the door for nonprofit hospitals to retain tax-exempt status without caring for indigent patients and, later, to pocket profits from for-profit subsidiaries tax-free and to form partnerships with Silicon Valley venture capital firms.
AMCs are hospitals that provide patient care, educate health care providers in partnership with at least one medical school, and have a capacity for research and development of products and processes that improve patient health. AMCs have the capacity to treat the most complex health cases and to provide the highest quality medical care. They also tend to treat a wealthier and whiter population than nearby safety-net hospitals in urban areas. There is evidence that uninsured and Medicaid patients, who are disproportionately racial and ethnic minorities (KFF 2022), face barriers to obtaining care at AMCs (Tikkanen et al. 2017; Acosta and Aguilar-Gaxiola 2014).
Hospital venture capital arms typically receive investment from or partner with Silicon Valley VC firms.4 Investments by these venture capital subsidiaries have increased substantially since 2010, with major increases during the COVID-19 pandemic. Total investments by the VC arms of major hospitals went from $284.53 million in 2010 to $2.7 billion in 2021, a tenfold increase (Pifer 2022).
Nonprofit hospital systems utilize a number of financial strategies to increase their nonoperating revenue in addition to venture capital investments. They held more than $283 billion in stocks, hedge funds, private equity, venture funds, and other investment assets in 2019 (Rau 2021). Only $19 billion, or 7 percent, of their total investments, were principally devoted to their nonprofit missions rather than producing income (Rau 2021). Where does this massive amount of nonoperating revenue come from? According to Becker’s Healthcare, at least 23 hospitals now have their own investment arms (Diaz 2023). The number of dollars funneled into venture activity by large hospitals in recent years dramatically outpaces what it was a decade ago (Figure 2 in Pifer 2022). Annual venture funding round activity in 2020 was $807.41 million for Kaiser Permanente Ventures (five times its 2010 investment), $626.6 million for Ascension Ventures (five times its 2010 investment), and $269.6 million for Mayo Clinic Ventures (three times its 2011 investment) (Pifer 2022).
Across the whole health care industry, recent top priorities of venture capital are to invest in health care data infrastructure providing software, hardware, or advisory services in the space (Balasubramanian 2023), as well as digital health, mobile health, health information technology, wearable devices, telehealth and telemedicine, and personalized medicine (Gondi and Song 2019). For example, the value of investments in digital health increased by 858 percent between 2010 and 2017, outdoing the 166 percent growth in total venture capital funding in the overall economy (Gondi and Song 2019). The pandemic certainly spurred investment in this area as well as in hospitals as health systems ramped up their virtual communications (Pifer 2022). As technology’s presence in health care continues to increase, venture capital firms will be there. Hospitals are not just the customers of new venture capital-led innovations but many are major investors, contributing their own funds.
Nonprofit hospitals are granted an exemption from paying taxes in exchange for promoting health and providing free or below-cost care to those unable to pay. Free care for indigent patients has been a basic tenet of charitable hospitals for centuries and has long been the basis for the tax exemption enjoyed by today’s nonprofit hospitals. A 1956 IRS standard said hospitals had to be “operated to the extent of [their] financial ability for those not able to pay for the services rendered and not exclusively for those who are able and expected to pay” (Rev. Rul. 56-185, 1956-1 C.B. 202). Essentially, charity care for uninsured or underinsured was required for hospitals to receive an exemption from paying taxes.
This established tax-exemption definition was drastically changed by a 1969 IRS revenue rule (C.B. 117. Revenue Ruling 69-545),5 which removed the stipulation that providing charity care for the poor was the only way to satisfy the tax-exemption requirement. The definition of charity care was broadened. Now hospitals were able to provide vaguely defined community benefits to retain their tax-exempt status: “A nonprofit hospital must be organized and operated exclusively in furtherance of some purpose considered ‘charitable’ in the generally accepted legal sense of that term, and the hospital may not be operated, directly or indirectly, for the benefit of private interests” (C.B. 117. Revenue Ruling 69-545, page 2). Ambiguous language left open an important question: was it now a condition of tax exemption that a hospital accept patients covered by Medicaid and Medicare? (Fox and Schaffer 1991, 258). Although a hospital was no longer required to provide charity care, the IRS said it considers doing so to be a significant factor indicating community benefit (GAO 2023). The change was a sharp turn from the centuries-old definition (Fox and Schaffer 1991). Fox and Schaffer (1991) argue that the 1969 rule made it easier for hospitals to refuse to treat Medicaid and uninsured patients.
As a result of the 1969 IRS ruling, hospitals can satisfy the community benefit requirement by paying for health promotion activities. Some nonprofit hospitals have interpreted this to include absorbing payment-cost differentials from public programs, community health improvement services, and operations, health professionals’ education, and research (IRS Schedule H 990 2023). The majority of community benefit spending still goes to uncompensated care (Young et al. 2013), but health-promoting activities and investments are a growing share.
The 1969 IRS rule did not establish a mechanism to check on whether hospitals are actually providing benefits to the community. The IRS does not have the authority to mandate these activities and federal law does not say how much and what type of community benefit hospitals have to provide; that power resides with Congress. Between 1969 and 1989, no hospital lost its tax-exempt status for failing to provide free emergency room care or serve Medicaid patients as the IRS had no program in place to monitor compliance. Finally, in 1985, Congress passed legislation – called the Emergency Medical Treatment and Active Labor Act6 – that required tax-exempt hospitals to provide emergency medical services regardless of the patient’s ability to pay. Furthermore, the IRS ruled that providing emergency services plus the acceptance of Medicaid patients were required to demonstrate charity care (Fox and Schaffer 1991:253-274).
Today, the IRS has six different factors that can satisfy the community benefit needed to maintain tax exemption (GAO 2023):
The Affordable Care Act set three further requirements for hospitals:
Nonprofit, tax-exempt hospitals are only reviewed by the IRS once every three years and have the flexibility to determine what counts as charity care and even how much they undertake to contribute to the community (GAO 2023). This ultimately means that nonprofit hospitals are technically only supposed to be sanctioned if they refuse to treat Medicaid patients or uninsured people experiencing an emergency medical situation (Fox and Schaffer 1991: 351-2). But in reality, the IRS does not follow through on sanctioning these hospitals nor does it have an organized, consistent data collection system. In a recent report, the Government Accountability Office analyzed 2020 IRS data and found 30 nonprofit hospitals that got tax breaks in 2016 despite reporting no spending on community benefits (GAO 2023).
The Kaiser Family Foundation estimated the total tax exemption for all nonprofit hospitals (including federal, state, and local taxation) was $28 billion in 2020 (Godwin, Levinson, and Hulver 2023). Federal tax exemption accounts for about half of this ($14.4 billion) while state and local tax exemption was $13.7 billion. Most nonprofit hospitals aren’t required to pay state or local sales taxes, local property taxes, or state corporate income taxes. However, there is some variation as states attempt to hold the hospitals accountable (Godwin, Levinson, and Hulver 2023).
The Lown Institute, a health care think tank, compared 1,700 nonprofit hospital systems’ spending on financial assistance and community investment to the estimated value of their tax exemption. This “fair share spending” measure puts a value on how much nonprofit hospitals are actually giving back to their communities. The report found that in 2023, 77 percent of hospitals spent less on actual care for the poor and community health investment than the estimated value of their tax breaks (Miller 2024).
Recent reporting indicates that some of the most profitable hospital markets in the country have the highest levels of patient debt (Levey 2022). Medical debt can be very high even in hospital systems that are thriving with large total margins, which begs the question of whether nonprofit hospitals are spending anywhere close to the value of their tax breaks. This charity care is vital for underinsured and uninsured people who bear a substantial part of the burden of medical debt. While the amount spent on charity care varies widely across hospitals, half of all hospitals reported that the cost of charity care represented just 1.4 percent or less of operating expenses in 2020 (Levinson, Hulver, and Neuman 2022). Additionally, research indicates that for-profit hospitals are spending just as much or more on charity care as nonprofit hospitals (as a percent of total expenses) despite the large tax breaks nonprofits receive (Bruch and Bellamy 2021).
There are a number of states modeling what federal legislative action can be taken to hold nonprofit tax-exempt hospitals accountable. We discuss the following two important case studies of Cleveland Clinic and UPMC.
When Congress passed the Balanced Budget Act in 1997, funding for nonprofit hospitals was cut so Medicare could rein in federal health care expenditures (Bazzoli et al. 2004-05). AMCs were among the recipients of this cut. The Act included large reductions in federal hospital payments (Appelbaum and Batt 2021) which reduced the revenue for hospitals that relied on Medicare reimbursements for patient care as a significant share of their income. At the same time, AMCs were also facing growing competition from large, consolidated hospital systems capable of treating mid- and high-acuity patients at lower costs.
As AMCs were struggling financially, a new possibility to raise revenue came along in 1998. An IRS ruling (Rev. Rul. 98-15) allowed nonprofit hospitals to own for-profit subsidiaries and pay no taxes on profits earned by these subsidiaries. This was an invitation for venture capital firms to partner with AMCs and other large nonprofit hospitals with a demonstrated research capability (e.g., Kaiser Permanente, Sutter Health, CommonSpirit) to develop patentable products and processes (Appelbaum and Batt 2021). The rule made it possible for nonprofit hospitals to benefit from the business activities of for-profit subsidiaries or joint ventures without paying taxes on the profit. The IRS permitted this type of alliance out of an initial concern that it was needed for AMCs to stay financially stable. Over time, however, it further enriched some of the most financially successful hospitals, exacerbating inequalities in access to resources for capital improvements and expansion. The advantages of nurturing start-ups whose profits are accrued tax-free by their AMC and Silicon Valley owners resulted in an explosive increase in investment income7 and CEO pay for the nonprofit hospitals (Liss 2019; Table 1 in Section 6 of this paper).
The large investment income of AMCs has enabled them to recruit the most skilled specialists in every field, to invest in state of the art technology, and in some cases to offer patients near luxury hotel accommodations and services. But oftentimes residents of the very poorest areas of the city with high rates of chronic disease and other health problems are unable to access AMC care, even if they live near the hospital, because it is not an emergency and they lack insurance coverage the AMC accepts. AMCs’ large nonoperating revenues have also fueled the consolidation of hospitals and health systems as these health systems have sufficient resources and/or access to borrowed funds to acquire other health providers.
When for-profit subsidiaries grow large enough to threaten the hospital’s nonprofit status, they can be spun out as for-profit, tax-paying corporations in which the hospital is a major shareholder. As a shareholder, the hospital will receive dividends. This is passive income on which the hospital is not required to pay taxes.
Case Study: Cleveland ClinicThe Cleveland Clinic, based in Cleveland, Ohio, is one of the most prominent academic medical centers and research institutions in the country. Most do not know it also has an active venture capital arm that generates billions of dollars annually. The Clinic has 80,642 caregivers, 23 hospitals, and 276 outpatient facilities in locations around the globe and is a major beneficiary Some of the greatest health disparities in Ohio are in the neighborhoods that directly surround the Cleveland Clinic. The two nearest neighborhoods, Fairfax and Hough, which are 95 percent African American, are poor and have high rates of poor health outcomes (Diamond 2017). They are two of the communities heavily impacted by redlining in the 1930s in Cleveland, the effects of which persist today (Wizner 2023). This is a community that relies on Medicaid and charity care. However, the payer mix by gross patient service revenues at Cleveland Clinic for most of 2023 was just 13 percent Medicaid patients, 33 percent Commercial, 51 percent Medicare, and 3 percent self-pay (Cass 2023). The Clinic boasts of the numerous community benefits it provides, including bringing jobs and increased economic activity to the city. But for many residents, this isn’t enough. Those in The tax-exemption policy the IRS put in place back in 1969 was intended for institutions that don’t make a profit like schools, hospitals, religious places, which are a public good, and therefore the public supports them. Today in 2024, Cleveland Clinic and other large academic medical centers are not struggling nonprofits pinching pennies. As tax-exempt, wealthy institutions that have used their resources for expansion and investment in for-profit subsidiaries, it is unfortunate that charity care and community benefit spending has stagnated or declined (Kacik 2020). While low-income residents of the neighborhoods surrounding Cleveland Clinic pay their property taxes, Cleveland Clinic is exempt from paying taxes on the $2.4 billion in property it owns (as of 2018) across the county (Allard 2024). This would translate to roughly $84 million annually in revenue for the government (Czekalinski and Indriolo 2022), money that would go towards the city and its communities’ schools, roads, and much more. |
Cleveland Clinic is not alone in creating a venture capital arm to build additional revenue streams while maintaining its tax-exempt status. At least 23 nonprofit and for-profit hospitals have investment arms (Diaz 2023), including the nation’s top ranked hospital, Mayo Clinic (Mayo Clinic Ventures & Mayo Clinic Platform), UPMC in Pittsburgh (UPMC Enterprises), and Northwell Health in New York state (Northwell Holdings). All three are nonprofits.
Numerous academic medical centers across the country are failing to adequately treat indigent patients and provide full community benefits while making lots of money and rewarding their CEOs handsomely. This is a failure of IRS tax enforcement to properly oversee these hospitals’ nonprofit status.
The University of Pittsburgh Medical Center (renamed UPMC in 1990) is another example of an Academic Medical Center that has strategically used its for-profit subsidiaries to amass income. However, the workers, surrounding community, and Medicaid/uninsured patients who access UPMC have not experienced the benefits of the wealthy system despite being in their backyard.
UPMC has been actively engaged in the acquisition of hospitals since the mid-1990s. UPMC’s large venture capital investment arm and exemption from paying taxes has fueled its expansion. Originally just three university-affiliated hospitals that merged in 1990, it is now a health care giant and insurer with 92,000 employees across 40 hospitals and an operating revenue of $26 billion.
Case Study: UPMCUMPC has taken full advantage of loose regulations governing nonprofit hospitals to amass millions of dollars in profits, build its footprint in Pennsylvania, and destroy competition by buying up other facilities. It is now the biggest employer and hospital system in Allegheny County, where Pittsburgh lies. With monopolization and consolidation of hospitals comes price inflation for treatment and procedures, reduced worker power, and lower-quality patient care. According to the Lown Institute, UPMC was the least charitable nonprofit in the country (Miller 2024). They are exempt from all federal, state, and local taxation. UPMC took in $246 million more in tax breaks than it spent on charity care and community investment in 2023 (Miller 2024). Meanwhile, UPMC CEO, Leslie Davis, made $4.2 million in fiscal year 2022 (Internal Revenue Service, UPMC 990 form, 2022). For years different members and stakeholders of the Pittsburgh community have critiqued UPMC’s nonprofit tax-exempt status. Last year, city officials, led by the sitting mayor, began UPMC Enterprises is the venture capital arm of the health system and invests in UPMC Enterprises has 172 different coinvestors in different investment ventures. It has entered into deals with 4BIO Capital, Altitude Life Science Ventures, First Trust Capital Partners, Foresite Capital, Innovation Workers, and Jeito, among other venture capital firms. The venture capital firms UPMC works with are in biotech, financial services, health care, robotics, artificial intelligence, medical devices, retail technologies, and enterprise software. The majority of UPMC’s investment activity is in the venture capital space but it also has made deals and acquisitions with private equity companies (Q-Centrix, Butterfly Network, Hashed Health, and CarepathRx) in recent years. Like Silicon Valley VC firms, VC subsidiaries of hospitals sell start-up companies when they mature. In June 2024, UPMC sold its inpatient virtual consulting technology to health tech vendor eVisit. As UPMC is the largest health care provider in the state, patients are likely to need care at its facilities and workers are likely to be employed by its hospitals. It has been a union-busting employer since its start. SEIU Healthcare Pennsylvania, which is the largest health care union in the state, has long tried to organize a union with workers at UPMC facilities. Workers have continuously been met with threats of termination for their organizing activities, and there are many other counts of unfair labor practices (Deto 2021). In May 2023, SEIU Healthcare Pennsylvania and other major labor unions filed an antitrust complaint against UPMC with the Department of Justice. The workers asked the DOJ to investigate their charges that the hospital system uses its size and power in the state to wield monopsony power in the local labor market and hold down wages (Muoio 2023). The health system has also been subject to numerous National Labor Relations Board (NLRB) cases, most Not only does UPMC operate hospitals but it also runs one of the largest health insurance companies in the state, UPMC Insurance Services, that covers 4 million people. In 2020, the health plan contributed $11.4 billion of UPMC’s total $23.1 billion in operating revenue (Appelbaum and Batt 2021). But even workers at its own hospitals that are covered by its insurance complain that it is expensive and has minimal coverage. As many as 36 percent of UPMC’s workers said they are in medical debt to their own employer when surveyed for a complaint the workers filed to the Department of Justice. For low-wage staff at the hospitals it was 51 percent (Deto 2019; SEIU and SOC 2023). SEIU, which organizes health care workers across the country, says the medical debt of UPMC workers outpaces other facilities (Hamill 2022). UPMC’s health plan has long been in competition with Highmark Health, the other major health insurance plan in western Pennsylvania. Since 2011, both integrated systems have attempted to exclude their facilities from the other’s networks. The Attorney General of Pennsylvania alleged in 2019 that UPMC failed to limit amounts charged to Highmark subscribers, denied treatment to out-of-network patients, and refused to contract with Highmark and other health plans Community WoesCommunity grievances against UPMC go back years and have deep roots not just in Pittsburgh but across Pennsylvania. In the same period that UPMC bought out 28 new hospitals (1996 to 2019), it fully closed four hospitals and eliminated services from others. The Braddock community, which is a predominantly Black town in the eastern suburbs of Pittsburgh were devastated by the closure of its UPMC hospital roughly 15 years ago in January 2010. UPMC claimed that it was underutilized. The Braddock Council President at the time filed a complaint with the US Department of Justice claiming the closure violated Title VI of the Civil Rights Act. The US Department of Human Services Civil Rights Division conducted an investigation and community and labor activists in the area pushed to stop the closure (WTAE-TV Pittsburgh UPMC Pinnacle Lancaster Hospital closed in February 2019. In early 2020, UPMC Susquehanna Sunbury Hospital closed after more than 100 years of operation (Eble 2019). The closure was announced just 17 months after acquiring it. In early 2020, UPMC Susquehanna Sunbury At nearly every closed facility, UPMC promised that at least some employees would be moved In facilities where workers were not laid off due to closures, employees are struggling to do their jobs because of massive staffing shortages. UPMC dominates the hospital market for Pittsburg and much of Western Pennsylvania and according to workers, its policies drive this trend of understaffing and low job satisfaction. A whopping 93 percent of Pittsburgh hospital workers said they think about leaving their jobs at least once a month and 90 percent reported that The most recent large-scale acquisition UPMC carried out was of the nonprofit hospital, Washington Health Care Services (WHS), which officially went through on June 1, 2024 (Hudson 2024). The acquisition has been a major source of debate in Pittsburgh. The WHS board signed a nonbinding agreement of intent to negotiate an integration in June 2023 and the board of the hospital provided assurances that no staff would lose their jobs or have their pay and benefits degraded. If not for the merger, WHS said it would go bankrupt, a common rationale to persuade antitrust regulators to approve the merger. There are 2,000 employees across two WHS hospitals: a flagship 278-bed facility in Washington, Pennsylvania, and its 49-bed hospital in Waynesburg, Pennsylvania. These facilities will merge with UPMC’s existing 40-hospital footprint employing more than 100,000 staff (Halleman 2023). |
Large health systems with greater cash reserves and stronger assets were able to increase their investments during the time of acute financial uncertainty amidst the pandemic (Pifer 2022). Most of the largest venture capital deals from the past few years are from these larger actors. The access to funding that large health systems have widens the gulf between their quality of facilities and quality of care and other acute care hospitals that don’t have their resources.
As the examples of Cleveland Clinic and UPMC show, there is something very wrong with the definition of “tax-exempt” as it applies to many nonprofit hospitals, not least to AMCs. Countless communities across the country are not receiving the benefits that could be provided by requiring nonprofit hospitals to treat underinsured and uninsured patients in order to maintain their exempt status. Taxing well-endowed, rich academic medical centers and other wealthy nonprofit health systems on the profits, above a threshold, of their for-profit subsidiaries would raise substantial sums for cash-strapped cities and rural areas. Some of this momentum is already building among Congressional members; last year, a bipartisan group of Senators including Elizabeth Warren (D-MA) and Chuck Grassley (R-IA) sent letters to the commissioner of the Internal Revenue Service (IRS) and the Treasury Inspector General for Tax Administration calling for an investigation into “overly broad” tax wording and oversight of roughly $28 billion in exemptions (United States Senate 2023; Owermohle 2023).
More than a dozen states have passed or considered legislation to better regulate the tax-exempt status of nonprofit hospitals and define what types of charity care need to be offered (Miller and Hawryluk 2023). A tool from The Hilltop Institute at the University of Maryland Baltimore Campus (UMBC) provides a thorough breakdown of each state’s community benefit requirements and tax exemptions for nonprofit hospitals.8 A standard in Illinois (Section 15-86 of the Property Tax Code, established in 2012) limits the value of the state property tax exclusions to the amount a hospital provides in charity care (Section 35 ILCS 200/15-86). As of January 2020, Oregon required hospitals and affiliated clinics to subsidize care to patients with incomes up to 400 percent of the federal poverty level and provide completely free care to patients with incomes under 200 percent of the poverty level (Tiel 2019). There are many other innovative state approaches to holding nonprofit hospitals accountable that could be a model for other states or be adopted federally (Gee and Waldrop 2022).
On a federal level, a reconsideration by Congress of what it means to get tax breaks as a nonprofit hospital could provide poorer people access to the quality of care available only in AMCs when their health conditions warrant it. Taxation of profits generated by for-profit subsidiaries would reduce hospitals’ ability to acquire other hospitals and consolidate them in a single health system, with all the ills that consolidation brings. It would also increase tax revenues to state and local governments as well as the federal government.
There are concrete policy steps that can hold nonprofit hospitals accountable. The first is that Congress must tax all profits made by for-profit subsidiaries of nonprofit hospitals above a certain threshold. As we display in the case studies above, hospitals that operate their own venture capital firms or partner with these firms, generate massive wealth that far exceeds operating costs. Total investments by venture capital subsidiaries of hospitals were $2.7 billion in 2021, a large share of which was nonprofit hospitals. This must be taxed especially as academic medical centers ramp up their interest in leveraging VC arms to commercialize internally developed intellectual property (Pifer 2022).
Secondly, Congress should establish rules so the value of hospitals’ charity care is comparable to the amount of tax breaks they receive. Currently, five states (Utah, Texas, Pennsylvania, Nevada, and Illinois) impose minimum community benefit levels nonprofit hospitals must provide (The Hilltop Institute n.d.). The Texas Tax Code directs tax-exempt hospitals to provide community benefits that amount to at least five percent of the hospital’s net patient revenue and provide enough charity care and government-sponsored health care that it accounts for at least four percent of net patient revenue.9 In Illinois, nonprofit hospitals seeking a property tax exemption must provide charity care or other specified services or activities at levels at least equivalent to what the hospital otherwise would be required to pay in property taxes.10 Nevada law requires that nonprofit and for-profit hospitals that have at least 100 beds and are located in a county that has at least 2 licensed hospitals provide a specified minimum level of charity care.
Thirdly, Congress must establish clear, enforceable standards for nonprofit hospital financial assistance programs that dictate what income group is entitled to charity care. This is a recommendation that Senator Bernie Sanders promotes (2023). Twenty-four states limit hospital billing and charging practices for the welfare of low-income individuals, but the extent varies greatly. In Oregon, hospitals must provide subsidized care to any patients earning up to 400 percent of the federal poverty level and free care to any below 200 percent of the poverty level (Tiel 2019). Regardless of whether a patient proactively requests the financial assistance program or charity care they are entitled to, they will receive subsidized or free care. California limits the amounts hospitals may charge patients whose income does not exceed 350 percent of the federal poverty line (Sen et al. 2023)
Overall, a fifth of Americans live in rural areas although the share is much higher in some states. Vermont, with almost two-thirds (64.9 percent) of its population living in rural areas, has the highest share. The states with the largest number of rural residents are Texas (4.7 million), North Carolina (3.5 million), Pennsylvania (3 million) and Ohio (2.8 million). Millions of people depend on rural hospitals, defined as hospitals located outside of metropolitan areas, for care when they develop a serious illness or have an emergency that needs immediate medical attention (Census Bureau revised 2024).
Rural hospitals offer vital lifelines for their surrounding communities, due to the limited number of health care providers in remote areas. They also play a significant economic role in their communities. According to the National Rural Health Association (NRHA), they are typically the largest or second largest employer in these areas (Cary 2020). For women, they provide access to comprehensive care for themselves and their children as well as employment opportunities. More generally, for both the health and the economy of the communities they serve,they must be able to maintain and upgrade their technology and facilities. There is, however, very little serious research on hospitals’ capital investment projects, and even less that examines this for rural hospitals.
These hospitals face unique problems created by the geography, demography, and economy of rural communities. They face major challenges in staffing, financing, low patient volumes, and aging infrastructure. The small size, thin margins, and heavy reliance on Medicaid as payer puts these hospitals at a disadvantage in obtaining funding and finding funding for investment in the hospital’s physical infrastructure, like its buildings, labs, expensive mechanical systems, modern technology, and medical equipment.
Capital investments in the latest equipment, technologies, and renovations or replacing aging infrastructure are essential to assuring a hospital’s financial stability. These investments have positive effects on the efficiency of hospital operations and quality of care and are important in attracting doctors and patients. Rural hospitals have numerous capital needs. Many small rural hospitals were built in the era of HIll-Burton and now must deal with an aging infrastructure. They require funding for major capital projects to renovate or replace the physical facility, to implement new design practices to manage patient flow and improve infection control, and to purchase and implement key IT systems such as electronic health systems and telehealth systems. Installation and implementation can add significantly to costs (Rural Health Information Hub 2024).
Capital Investments also enable rural hospitals to meet the changing needs of their communities by investing in new services, such as outpatient facilities, or adding new lines of inpatient services that increase the patient population and revenue of the hospital. Capital projects can be expensive. Internal sources of funding such as profits and cash flow are important as a direct source of funds for capital investment. They are also important for obtaining external funding as they can be used to make interest payments and repay loans (that is, service the debt) on money they borrow (Kim and McCue 2008).
Using data from the early 2000s, Kim and McCue examined the market, operational, and financial factors that influence capital investment by rural hospitals. The data are scaled by hospital assets at the baseline to facilitate comparisons among hospitals. The factors expected to affect capital investment are grouped into three categories: market factors, operational factors, and financial factors. Among the specific factors the researchers examined in these categories: the size of the population over 65, the age of the physical structures, and liquidity-affected investment in facilities, and adoption of new technology. Liquidity is a measure of how quickly assets can be converted into cash. The over-65 population and liquidity had a positive effect on capital investment, while the age of the physical structures had a negative effect. A hospital with an aging physical plant may have difficulty attracting patients and clinicians and may find itself in a downward cycle. It will be unable to increase revenue and improve cash flow and will be unable to build internal cash reserves for capital projects and unable to access external funds by borrowing and taking on debt to finance capital improvements. Their physical structures, equipment, and technology will continue to age, compounding their lack of access to funds for capital projects and their ability to attract doctors and patients.
The theme of market dynamics and capital investments was taken up most recently by Beaulieu, Hicks and Chernew (2024). Using data from 2010/2012 (depending on data availability) to 2019, they investigate the market dynamics that link capital investments to changes in the volume of patients treated, market share, and prices. They identify a positive cycle in which hospitals that spend more on capital projects gain market share and raise prices while those that spend less lose market share and are less able to raise prices. As they describe it, “[t]aken together these forces perpetuate a cycle of expanding and withering hospitals” (p,2). Over time, this may lead to consolidation of rural hospitals as hospitals that fail to keep up are acquired by hospital chains. The higher prices partially reflect the higher quality of care associated with investment in modern facilities and technology and partially reflect an increase in the market pricing power of the consolidated chain.
Examining 2500 acute care general hospitals, the researchers found that investment in physical plant, equipment, and technology is a relatively small fraction of total expenses, typically 3.8 to 5.3 percent in the first year of the study. But capital expenditures for hospitals in the top 20 percent of spending on investments were two and a half times those in the middle 20 percent and more than six times those in the bottom 20 percent. In a rigorous and robust analysis, the researchers establish the positive relationship that capital investments have on the volume of patients a hospital treats and on its market share. Over the years from 2012 to 2019, patient volume and market share for hospitals spending the most on capital investment grew more rapidly than hospitals in the middle while the hospitals spending the least on capital expenditures grew more slowly than those in the middle. Hospitals are sorted into leaders and laggards in the growth of patient volume and market share, depending on their expenditures on capital, with leaders on a self-reinforcing upward trajectory and laggards on a self-reinforcing downward cycle.
The laggards fell behind because hospital management did not make capital improvements. It’s likely that a lack of internal funds (cash and financial assets that can be converted to cash) and external funds (borrowing in financial markets) was behind many of these decisions. Hospitals with low profits and low cash flow are not able to accumulate internal funds and will not be able to borrow in financial markets. What does this mean for rural hospitals?
The decline in profitability and the increase in financial distress of rural hospitals have become more pronounced in recent years. Using hospital data for the years 2010 to 2018, Carroll, Euhas, Beaulieu, and Chernew (2023) examine what happened to rural hospitals that were unprofitable in 2008–2010. They studied a sample of 858 rural hospitals, of which 325 were unprofitable. Two hundred and forty-three of these hospitals had no other hospital in a 15-mile radius, making their survival essential to the health of people in the communities they served. More than three-quarters (77 percent) of the 325 unprofitable hospitals remained open and free-standing in 2018, 7 percent closed, 4 percent merged with a nearby hospital, and 13 percent were acquired by hospitals or chains outside their local hospital market. More than half (56 percent) of the unprofitable hospitals that survived never became profitable in the years 2011 to 2018.11
Congress took note of the financial distress of rural hospitals and introduced the Medicare special payment classification program in an effort to stabilize their finances. This program consists of additional payments to certain rural hospitals provided by Congressional action in the 1980s and 1990s. Currently, there are four special classifications that a rural hospital can receive in addition to hospitals that receive the regular Prospective Payment System (PPS) described above in Section 3. The classifications are: Critical Access Hospitals (CAHs), Medicare-Dependent Hospitals (MDHs), Sole Community Hospitals (SCHs), and hospitals jointly classified as Rural Referral Centers (RRCs). Critical Access Hospitals are the backbone of rural health, accounting for about 58 percent of rural hospitals. Sole Community Hospitals account for 13 percent, Prospective Payment System hospitals for 12 percent, Rural Referral Centers for 11 percent, and Medicare-dependent Hospitals for 6 percent. These hospitals are eligible for higher reimbursement rates and payment adjustments intended to support them financially. Despite this, over half the rural hospitals that closed between 2005 and 2019 were classified as CAHs, MDHs, and SCHs. Rural hospitals paid under the PPS program accounted for the remaining bankruptcies (John, Malone and Pink 2022).
One reason for this is that the special benefits are tied to the hospital’s Medicare in-patient discharges. To be eligible for the special payments, hospitals are required to offer in-patient care. The size of the additional payments is based on the hospitals’ volume of Medicare discharges. But rural hospitals, like other hospitals, are increasingly providing outpatient services like health clinics, ambulatory surgery centers, home health agencies, outpatient physical therapy and rehabilitation services, and hospices. Indeed, outpatient services provide a higher share of revenue for rural hospitals as compared to urban hospitals: 74.2 percent compared to 52.3 percent in 2019, and is growing faster than in urban hospitals. In addition to patients’ increasing preference for outpatient care, residents of rural areas who require in-patient care and can afford it are seeking such care in hospitals with more modern facilities and up-to-date technology. The current system of supplementary payments may be out of sync and no longer the best way to help rural hospitals be profitable (John, Malone and Pink 2022).
Rural residents’ concerns that their local hospital may be behind in implementing modern technologies are not misplaced. A 2023 study of hospitals’ use of electronic health records (EHR), the technology most ubiquitously in use by hospitals for communication among their own doctors as well as with other hospitals, suggests that rural hospitals have fallen behind in implementing important IT technologies. Utilizing the American Hospital Association’s Annual Survey’s Information Technology Supplement, the researchers examined the general and routine use of EHRs by hospitals. Underscoring the complexity of achieving routine use of the full capabilities of this technology, the researchers found that the resources available to hospitals play a crucial role. Fifty-three percent of large hospitals reported routinely engaging in the broad use of EHR capabilities compared to 38 percent of small hospitals. In 2023, about 40 percent of rural and critical access hospitals (CAHs) were still not up to speed in the use of this technology and could not engage in its routine use (Gabriel, Richwine, Strawley, Barker, and Everson 2023).
What happens to the rural hospitals that are unprofitable? They have four options. (1) They can close their doors, causing rural populations to lose access to vital health services. Shuttering a hospital in a rural area deprives it of a major economic anchor for the community and the loss of jobs and income can be disastrous for the area with spillovers to neighboring communities. (2) They can merge with a nearby hospital, preserving access to inpatient and outpatient services that are vital to the population they serve and preserving jobs that are essential to the local economy. But the merger may decrease competition and raises the specter that the market power that accompanies consolidation will lead to higher prices for procedures. Stringency of state merger regulations affect outcomes with respect to pricing and access. (3) Unprofitable rural hospitals can be acquired by a hospital, possibly part of a multi-hospital health system, that is out of their hospital service area. The target hospital is typically failing financially, has an aging physical plant, and has very little bargaining power. The acquiring hospital may see the merger as extending its footprint and providing an opportunity to increase revenue by consolidating the more profitable service lines of the acquired hospital in its own hospital. Post-merger, the acquired hospital (the target hospital) typically decreases services provided, cuts staff and employment levels, reduces costs, and increases capital expenditures. Mergers of hospitals in different health care markets do not directly affect prices charged for procedures, but they can affect access by deciding which services will be available locally and which will require patients to travel longer distances to receive them (Williams et al. 2020).
Fourth and importantly, there is a very large share of hospitals, more than half in the Carroll, Euhas, Beaulieu, and Chernew (2023) study, that were unprofitable from 2008 to 2010 and were still functioning from 2016 to 2018, with more than half of these never returning to profitability over that time period. Without profits to build up reserves so they can fund modernization and expansion internally or attract investors who will lend them funds to finance expansion externally, they are trapped in a downward cycle. These are the hospitals the researchers identify as withering.
Some hospitals that were unprofitable at the start of the study and returned to profitability may have been able to access public programs that support capital investment by rural hospitals (Rural Health Information Hub n.d.). The US Department of Agriculture’s (USDA) Rural Economic Development Loan and Grant Program (REDL and REDG) supports rural economic development and job creation programs. It provides financing of medical facilities and equipment to provide care to rural residents and encourages the development of new providers by financing start-up costs for fixed assets such as real estate, new or existing buildings, equipment, or working capital. These grants and loans typically do not cover the full costs of capital projects, requiring rural hospitals to cobble together financing by applying for additional loans to agencies like the Small Business Administration (SBA), a complex and daunting task for an understaffed rural hospital. The Department of Housing and Urban Development (HUD) provides loan and mortgage insurance through Hud Section 242’s Hospital Mortgage Insurance Program. The program guarantees to lenders that HUD will pay all or most of an outstanding loan if the hospital defaults. The loans can be used to help rural hospitals, including Critical Access Hospitals, with the costs of remodeling, expansion, modernization, equipment, refinancing, and acquisition. To qualify for HUD loan guarantees, hospitals must be able to show that they will be able to repay the loans, something most unprofitable hospitals would likely have difficulty doing.
The slow pace at which struggling, unprofitable rural hospitals are closing provides an opportunity for policymakers to intervene and preserve access to health services and hospital jobs in rural communities. Carroll, Euhas, Beaulieu, and Chernew (2023) propose that policymakers adopt a new approach to antitrust regulations that recognizes that acquisition by a stronger hospital may be a rural hospital’s only chance to continue serving its community. The researchers urge caution in applying this new approach so that it cannot be gamed by large, well-resourced hospital systems.
Case studies suggest there are problems with using Certificates of Public Advantage, or COPAs, for the acquisition of a hospital by a local competitor. There are also problems with allowing acquisition by a stronger hospital system outside the target hospital’s health area. We illustrate with two examples.
Memorial Mission Hospital was founded in Asheville, North Carolina in 1885. Over the next hundred years, it merged with Biltmore Hospital, Norburn Hospital, and the Asheville Colored Hospital (Posner 2015). A century later in the early 1990s, its flagship hospital, Memorial Mission Hospital – Asheville had grown to 381 beds. The hospital competed head-to-head with St. Joseph’s Hospital, a 265-bed hospital and the only other acute care hospital in the city of about 830,000 people. By 1993 the two mid-sized hospitals wanted to form a partnership. Concerned that federal regulators would interfere, the hospitals lobbied the North Carolina General Assembly to enact a Certificate of Public Advantage (COPA) law. In 1994 federal antitrust regulators opened an investigation into the growing partnership of the two hospitals. The worry was that the combination of Mission and St. Joseph’s would result in a single large hospital system that could use its dominant position to raise prices. In 1995, the two hospitals applied for a COPA to shield their collaboration from federal antitrust challenges. That year the COPA took effect with a signed agreement between the hospitals and the state of North Carolina (Berenson and Bovbjerg 2015; Davis v HCA, 2021).
State laws called COPAs, address the situation where hospital mergers lead to cost efficiencies that provide more value than competition would. To limit risks of rising prices due to monopoly power, COPAs are subject to state oversight. In the Mission – St. Joseph’s hospital merger, the COPA imposed conditions that the state believed would protect patients against an increase in prices and would assure that they continued to have a choice of doctors. The regulations set by North Carolina for the consolidated Mission Hospital contained three constraints (Certificate of Public Advantage 2011; Vistes 2011).
1. Cost caps: Under the COPA, the rate of increase in Mission Hospital’s “cost per adjusted patient discharge” must not exceed the rate of increase in the producer price index for general medical and surgical hospitals in the US.
2. Margin caps: Under the COPA, the operating margin of the Mission Health System over any three-year period must not exceed by more than one percent the mean of the median operating margin of comparable hospitals.
3. Physician caps: Under the COPA, the Mission Hospital System is not permitted to employ, or enter into exclusive contracts with, more than 30 percent of the physicians practicing in Buncombe and Madison counties except those practicing in cardiology, genetics, neurology, or as hospitalists.
COPAs such as Mission’s, block federal antitrust enforcement and substitute state regulation. The caps were intended to limit price increases and reduce incentives for consolidation.
The Mission COPA operated for years without much controversy. Mission self-reported its compliance in annual reports that were reviewed by state agencies and experts they called in. Funding for the state oversight was relatively modest, with a maximum of $25,000 in annual fees payable by Mission Health (Fuse Brown 2019). Over the years, despite the COPA, Mission grew from two mid-sized hospitals into a multi-hospital health system with five hospitals in rural counties in western North Carolina, multiple clinics, and many physician practices. It became the dominant hospital system in that part of the state.
It was not until 2010 that questions about Mission’s growth and the advantages it received from the COPA were raised, and competitors made demands for changes in state regulations. Complaints by physicians and other hospitals about rising prices and charges to insurers led to a 2011 investigation of the system by the North Carolina legislature. The investigation found price increases of at least 20 percent above increases in prices in control groups of hospitals; it also heard employees’ reports of layoffs and cuts in pay. Additionally, the investigation report pointed out that the specific formula of the North Carolina COPA unintentionally created incentives for Mission to acquire outlying hospitals because the cost and margin caps only applied to the Asheville hospital’s location (Vistnes 2011).
In the end, the investigation was inconclusive. A lack of transparency on Mission’s part and competing claims by experts made it difficult to evaluate Mission’s economic behavior.
Nevertheless, in the wake of the investigation, Mission Health’s leaders lobbied the North Carolina General Assembly to repeal the COPA law. Mission’s CEO, Dr. Ron Paulus, argued that the COPA “has outlived its useful life” (Barrett 2015; Fuse Brown 2019). Mission succeeded. In September 2015, the General Assembly repealed the law.
After the COPA was repealed, the adverse consequences of consolidation and monopoly pricing emerged. Mission became aggressive in how it negotiated with health insurer Blue Cross, ultimately dropping the insurer from its network when the insurer did not accede to its wishes for high reimbursements (Hoban 2015). In addition, the health system engaged in improper restraints on competition by enforcing unlawful terms and arrangements with private payers, including commercial health plans, and third-party administrators of self-insured plans. These improper restraints included all-or-nothing arrangements, gag clauses, and other anticompetitive terms. These anticompetitive acts increased the prices of hospital services, insurance premiums, and copays or deductibles paid by residents of Mission’s overall 18-county western North Carolina service area (Davis v HCA 2021).
The COPA’s repeal created a regulatory void in state oversight that allowed the hospital system to become an unregulated monopoly and position itself for sale to Hospital Corporation of America (HCA), the largest US for-profit health system. The sale was finalized in January 2019 (Fuse Brown 2019). HCA already owned hospitals in western North Carolina that competed with Mission in Asheville and in rural areas. Post-acquisition, HCA became the largest employer and largest corporation in western North Carolina. It also became the monopoly provider of acute care services, with a 90 percent market share for inpatient care in three counties and between 75 and 90 percent share in four others (Davis v. HCA 2021: 4).
Not until a class-action lawsuit, Davis v. HCA, was filed on August 10, 2021, by citizens in seven western NC counties served by Mission/HCA Healthcare did the facts about Mission health system’s anticompetitive behavior become clear. According to the complaint, HCA bought the Mission system “precisely because of Mission’s outsized ability to dictate prices and other contract terms to its customers” (Davis v. HCA 2021:6).
The Mission Health COPA failed. It did not hold down health care costs and it permitted Mission to grow into a monopoly with the ability to exercise market power in setting prices. As a major health provider and employer in rural areas, the health system is able to lobby successfully and affect the decisions of state legislatures. A better-designed COPA might have constrained Mission’s behavior. But, it could not overcome the basic premise of the COPA — state-facilitated consolidation of hospitals and monopoly pricing power. The full impact only becomes clear when the COPA expires or is rescinded by state authorities.
Two of the largest health systems in the country – Scion and Lifepoint – are owned by the private equity firm Apollo Global Management. Together, their footprint is 220 hospitals across 36 states; they employ 75,000 people (Private Equity Stakeholder Project 2024). It owns the most rural hospitals (71) of any private equity firm (Gliadkovskaya 2023). Private equity ownership of hospitals has steadily increased over the past decade and is a harmful development for patients’ quality of care (Tkacik 2023), patients’ costs, local economies, and workers employed at the hospitals. Apollo’s Lifepoint and Scion hospitals provide examples of this.
Apollo formed Lifepoint and Scion from a series of acquisitions starting in 2018 when Apollo bought Lifepoint. Apollo then merged it with another hospital chain (RegionalCare Hospital Partners) and, most recently, acquired the large long-term acute care hospital chain Kindred Healthcare. This latter transaction also led to Lifepoint shifting a segment of the facilities and its existing hospitals into a new company called ScionHealth (Private Equity Stakeholder Project 2024).
Since 2018, Apollo has consolidated health care markets by rolling up rural and long-term health care providers. The hospitals it operates have had significant problems in care delivery, wage theft, and mistreatment of workers. Multiple Lifepoint facilities rank among the worst in their states (Private Equity Stakeholder Project 2024).
LifePoint cut operating costs substantially in 2020. The health system slashed salary and benefit costs by $166 million, cut supply costs by $54 million, and cut the charity care it provided by 21 percent compared to the previous year (O’Grady, Bugbee, and Fenne 2023). These cuts directly led to diminished quality of care at hospitals it owns. The health and safety of patients at a rural North Carolina Lifepoint hospital was endangered to the extent that regulators threatened to shut the hospital down. At another hospital in rural Wyoming, Lifepoint cut the services and staff so much that most were ultimately transferred to another LifePoint hospital 30 miles away. As a result, air ambulance utilization increased by 6 times over just 5 years (O’Grady, Bugbee, and Fenne 2023). At a hospital in New Mexico operated by Lifepoint, roughly 12 cancer patients, both insured and uninsured, have had their chemotherapy treatments denied, despite an agreement the hospital signed with the city and county that all oncology services are covered. The next closest hospital with an oncology center is four hours away (Morgenson 2024).
Apollo, the owner of Lifepoint, has cut OB/GYN services in favor of more lucrative services across many of its facilities, particularly in rural areas, thus exacerbating maternity and pediatric care deserts. This denied women served by these hospitals of the health services most important to them (Private Equity Stakeholder Project 2024). A rural Pennsylvania Lifepoint hospital ended all scheduled obstetrics deliveries because there was not “enough demand” for the services (Private Equity Stakeholder Project 2023).
As these examples show, the acquisition of failing hospitals by stronger ones, whether by hospitals in their health market or those outside this market, is fraught with possibilities for consolidation and higher prices or reductions in access and cuts in services and jobs. Antitrust regulators need to be cautious in viewing these potential solutions to the closure of rural hospitals. Still, they may need to take a more nuanced approach to the acquisition of weaker rural hospitals by larger chains, especially nonprofits, as these may save the hospital from closure, improve quality, and enable the hospital to return to financial stability. Consolidation can work to the advantage of patients and communities if strong regulations and oversight are in place to tamp down the negative effects of monopolization in rural health markets.
In the end, market solutions may not be the best solutions for rural hospitals. It may be time to consider a twenty-first century Hill-Burton Act focused on rural counties that have lost or are in danger of losing their local hospitals. The benefits of public funding of investment in hospital infrastructure, whether by government or philanthropy, are illustrated in the study of the large-scale investment in hospital infrastructure in North Carolina discussed earlier in this article. The investments in the physical plant were supported by the Duke Endowment, and the initial positive effects on health from improving capacity to care for patients were present decades later (Hollingsworth, Karbownik, Thomasson and Wray 2024).
The Coronavirus Aid, Relief, and Economic Security Act (CARES Act) was an urgent and important response by Congress to the economic and public health crisis wrought by the COVID-19 pandemic. However, the formula for distributing funds disproportionately favored wealthier hospitals. The pandemic was announced in March 2020, and by April 10, the Department of Health and Human Services (HHS) released the first phase of funding. The formula for distributing these funds to health organizations, overseen by Trump’s Treasury Secretary and designed by the Trump administration’s HHS, determined how much CARES Act relief hospitals received. Many safety net hospitals and rural hospitals were left unsupported.
During the first and largest phase of COVID-19 stimulus funding, $50 billion dollars of relief was allocated to hospitals and other provider organizations through a general distribution of funds by the Health Resources and Services Administration (HRSA). HRSA allocated $30 billion based on the organization’s or clinician’s share of total Medicare fee-for-service reimbursements in 2019 (Ellison 2020). The remaining $20 billion was allocated to hospitals based on the hospital’s net patient revenue in 2019 (Liss 2020). The general distribution was not based on a hospital’s need for resources to address the pandemic and hospitals and other recipients were not required to use these funds for treating patients. Based on these formulas, the wealthier hospitals, where patients were more likely to be covered by Medicare or private insurance, received more funds than safety net hospitals and community health centers, where patients are more likely on Medicaid or uninsured (Abramson 2020). Private insurers often pay nearly double what Medicare pays for all hospital services (Lopez, Neuman, Jacobson, and Levitt 2020). Notably, the formula did not take into account whether the hospital treated large numbers of COVID-19 patients and did not require hospitals to use CARES Act funds for their care. The first phase of funding came with no strings attached.
High reimbursement can come from having more privately insured patients coming through the door or being able to charge higher rates to private insurance companies because of their market power. If a hospital dominated the market at the point of the HHS funding, they were likely to do well with the formula. A Kaiser Family Foundation study found that hospitals with the lowest share of revenue from private insurance received half as much per hospital bed as their counterparts with the highest share during the first $50 billion general distribution wave of CARES Act funding in April 2020 (Schwartz and Damico 2020).
Wealthier hospitals with higher levels of Medicare reimbursements, higher private pay patients, or higher prior net revenues received emergency funding from the Provider Relief Fund (PRF) far more than did hospitals with greater need, i.e., those relying on Medicaid or serving rural or lower-income communities. The top 10 percent of hospitals based on share of private insurance revenue received $44,321 per hospital bed. They were more likely to be for-profit institutions, had larger operating margins, were less likely to be teaching hospitals, and provided less uncompensated care (a.k.a. charity care) (Schwartz and Damico 2020). The two largest hospital chains, HCA Healthcare Inc. and Tenet Healthcare Corp., both of which own hundreds of hospitals, received $5.3 billion and $2 billion in loans and grants, respectively, in the first wave (Terhune 2020). Within months, HCA returned to strong financial health with stocks soaring and 38 percent higher profits than the previous year (Abelson 2020). The chain ultimately returned a large portion of its relief (Pifer 2020). Along with Kaiser Permanente, it was one of the few wealthy hospital systems to do so.
Table 1
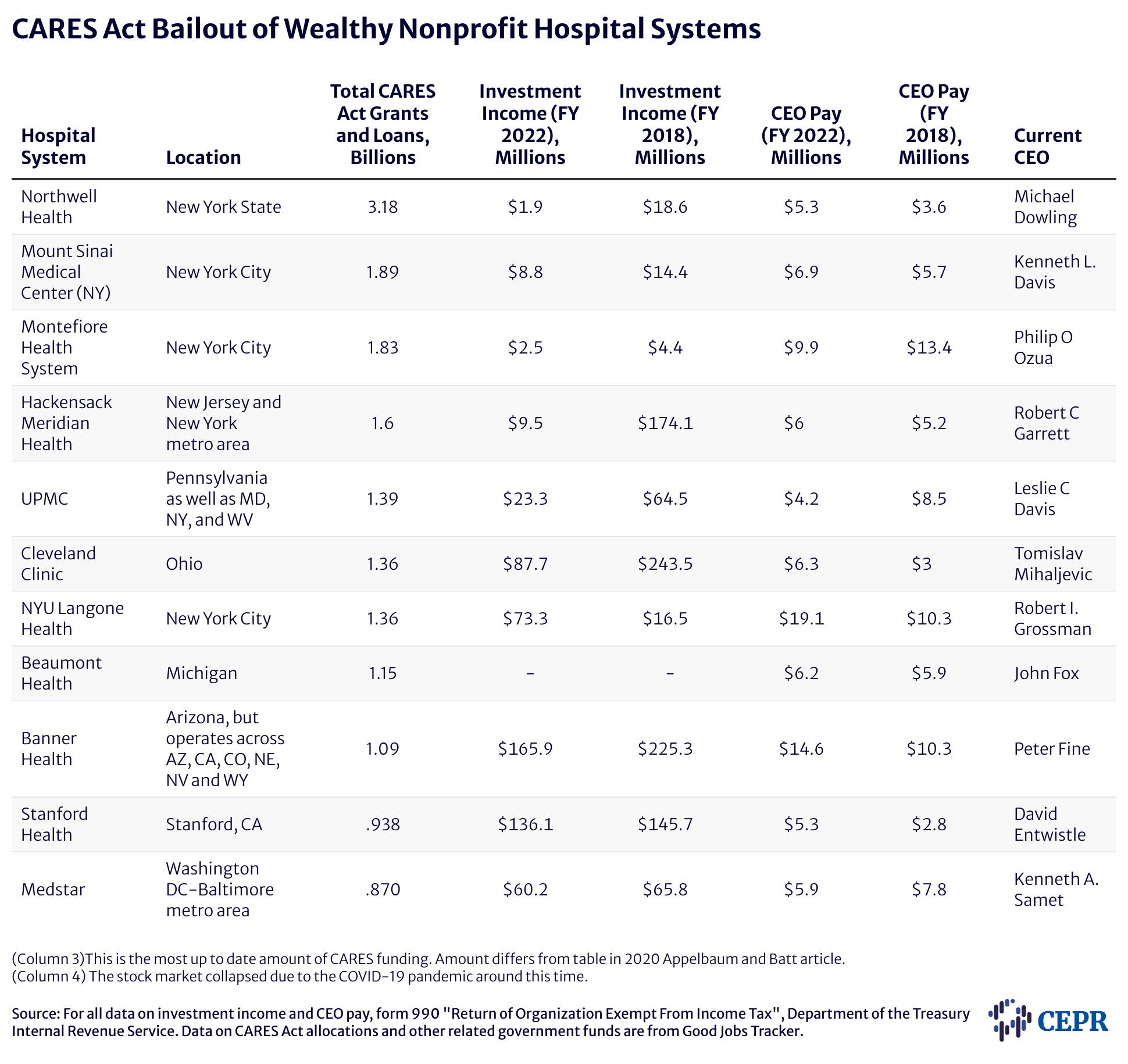
Meanwhile, hospitals and community health centers that serve poorer populations and receive most of their revenue from Medicaid, as opposed to Medicare and private insurers, went without or received very little of the initial $50 billion CARES Act funding pot. On average, they received just $20,710 per hospital bed. Only $2.6 billion of the $50 billion paid out went to Medicaid and CHIP providers. However, many of these institutions were either in rural areas or poor urban communities where COVID-19 infection rates were higher than in the geographies served by wealthy hospitals (Schwartz and Damico 2020). The disparity in revenue sources of these two groups of hospitals over many decades has led to financial instability of the hospitals serving most of America’s poorest communities. These are the hospitals that were inundated with COVID-19 patients in the early days of the pandemic. And, these are the hospitals that, in the immediate aftermath of the pandemic, received the least CARES Act funding to meet the challenge.
Academic Medical Centers typically have access to a safety net of financial resources that, ironically, safety net hospitals do not. Wealthy donors, endowments, and investment income enabled these and other well-endowed hospital systems to build substantial reserves. Despite this disparity in financial resources, CARES Act funding still favored hospitals that could more easily sustain the economic blow of the pandemic (see Table 1). Research shows that hospitals with significant cash on hand received more CARES Act PRF funding per bed than did hospitals with negligible cash available. While hospitals with at least 76 days of cash on hand received $88,000 per bed, hospitals with less than a week of cash on hand received $22,000 per bed on average (Grogan et al. 2021).
Pushback from public health experts and others led to reforms in how later rounds of PRF funds were distributed. The targeted allocations that passed in May 2020 made funds available to hospitals that were most impacted by COVID-19, including smaller and financially strapped community hospitals as well as large academic medical centers with high COVID-19 caseloads. These are the relief targets and amounts: a $20.7 billion “high-impact” fund intended for hospitals hardest hit by COVID-19, $10.9 billion to rural providers, $13.1 billion to safety net hospitals, $4.8 billion to skilled nursing facilities, $4.7 billion to nursing home infection control, quality, and performance, and finally $1.6 billion for children’s hospitals and tribal health providers (Coughlin 2022). For the targeted funding based on COVID-19 prevalence, academic-affiliated hospitals with higher assets prior to COVID-19 and hospitals that had higher numbers of COVID-19 cases received higher levels of funding. Yet again, the smaller critical access hospitals received lower levels of financial assistance per bed than their wealthier counterparts (Cantor et al. 2021).
Some hospitals, mainly rural hospitals and those serving poor communities, were missed in the first three general distribution phases of CARES Act distributions and high-impact distributions. This inequity was addressed to a greater extent in the fourth and final distribution of PRF funds which allocated an additional $8.2 billion to these hospitals in the new Biden administration’s American Rescue Plan (ARP). This was less than a year after the start of the pandemic and was an improvement from early rounds of stimulus. However, the disparity in nearly all the rounds of CARES Act funding came on the heels of years of unequal funding of U.S. hospitals.
Table 2
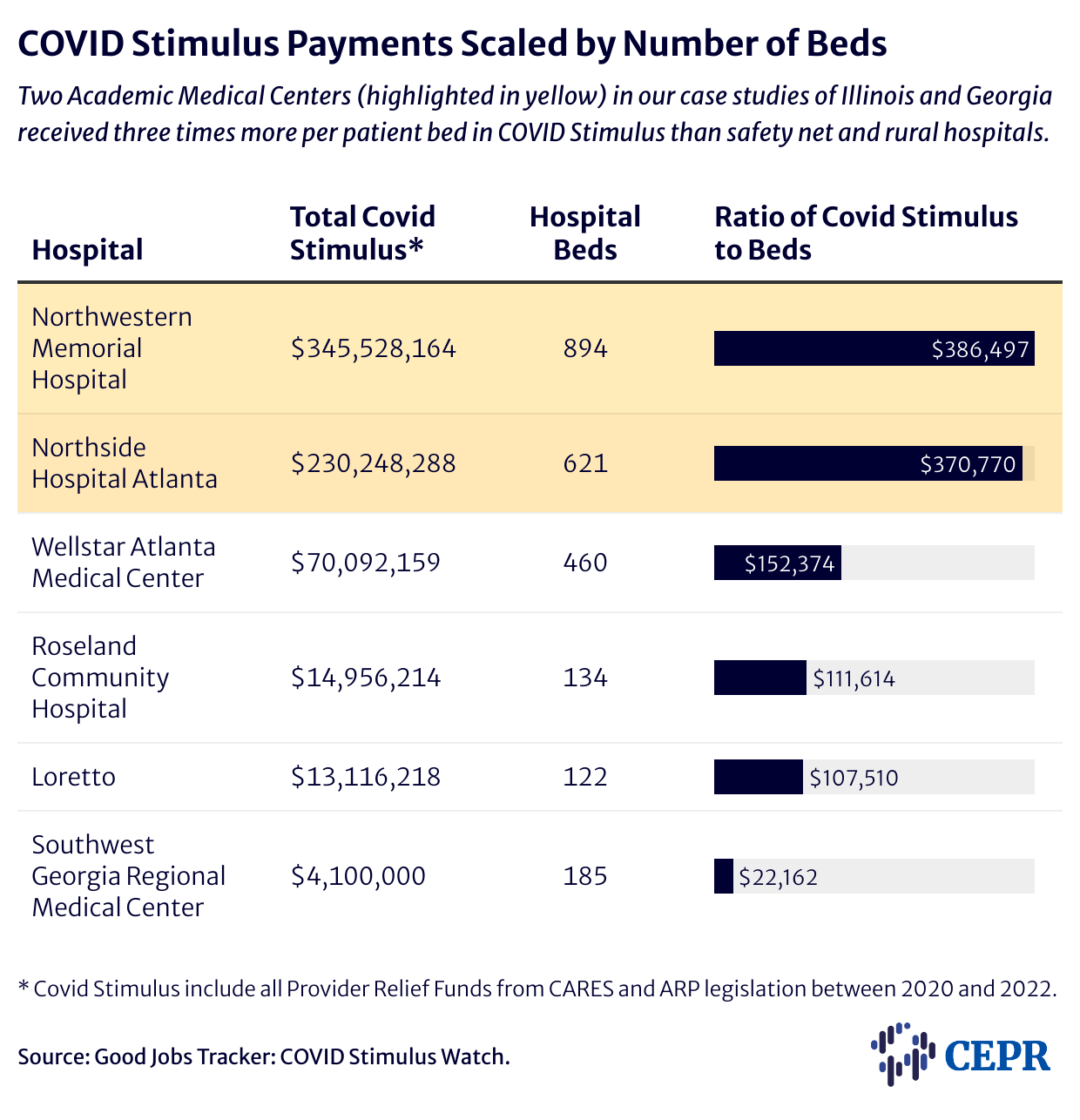
Table 2 displays the COVID Stimulus provided to hospitals in our case studies below in relation to the number of hospital beds at each.
We illustrate the effects of inequities in funding on health outcomes of COVID-19 patients by examining the allocation of CARES Act funds to two states: Georgia and Illinois, and the life and death effects for patients.
The availability of health care resources a facility had to treat COVID-19 patients played a major role in patients’ health outcomes and whether they survived the virus. Counties with lower staffing levels were associated with higher COVID-19-related deaths (Epané 2023) as were hospitals whose physical plant included fewer intensive care unit beds (Janke et al. 2021). It mattered where you lived and which hospital you had access to. Counties with higher per-capita incomes tended to have better resourced health care facilities and thus lower COVID-19-related deaths (Epané 2023). Black, Latino, and Native American people died at much higher rates than white people (Hill and Artiga 2022). Residents of rural communities also suffered higher rates of COVID-19-related deaths than did urban residents. Initially, urban counties had higher rates of COVID-19-related deaths, especially at the pandemic’s start. However, recent analysis shows that over the long term, patients from rural counties experienced higher mortality rates and tended to be readmitted more frequently following COVID-19 hospitalization (Yousufuddin 2024).
A total of $3.2 billion in CARES Act relief was allocated to Georgia as of early December 2020. Around 40 percent went to just 20 providers, leaving the more than 10,000 providers and facilities in the state to share the remainder (Shakoor, Gee, Rapfogel 2020). The story of how CARES Act relief was distributed in the state shows a disparate underinvestment in urban safety net and rural hospitals. This led to many Georgians lacking access to quality care and, in some cases, facing hospital closures in the middle of a pandemic. Georgia lawmakers’ decision not to adopt the Medicaid expansion in the Affordable Care Act (Obamacare) is a big part of the story as well.
Southwest Georgia Regional Medical Center in Cuthbert, Georgia closed just months into the COVID-19 pandemic. Suddenly, 6,400 people in the majority Black Randolph County where Cuthbert is located, lacked an emergency room, nursing home, and family medicine clinic (Bailey 2023). Randolph is in the bottom 10 counties in Georgia for patient health outcomes and had some of the highest COVID-19 case counts across the state. A third of county residents live in poverty and the median household income is $24,638 a year (US Census Bureau).
When cases spiked in the first month of the pandemic, Southwest Georgia Regional Medical Center lacked sufficient medical necessities and PPE, had no ventilators, and the air systems were not set up to create negative-pressure rooms (Berard 2020). Suddenly, 15 percent of the 200 staff were sick or unable to come in and the only reinforcements the state sent were six nurses and two respiratory therapists. By April 2020 just a month into the pandemic, Randolph County had the highest non-metro COVID death rate in America (Georgia Public Broadcasting, “The citizens of Cuthbert, Georgia…”).
The company that managed the hospital, Phoebe Putney Health System, declared to the city of Cuthbert that the hospital would not be providing COVID testing and did not have the ability to accept COVID-19 patients. It funneled infected patients to a facility an hour away in Albany, Georgia where Phoebe Putney manages a larger hospital. This larger Albany hospital had received $89.7 million in CARES Act provider relief whereas the Southwest Georgia Regional Medical received just $4.1 million (Goldhill 2021). COVID-19 infections required prompt attention so the lack of a local hospital meant life or death for some Cuthbert community members. In the two counties that the Southwest Georgia hospital served, Randolph and Terrell, one in every 200 people died from COVID-19. This death rate was 2.8 times that of all of Georgia (Goldhill 2021).
The relief provided to Southwest Georgia Regional Medical Center from the CARES Act was not enough. After 70 years of operation, the Medical Center officially closed in October 2020. According to the Mayor of Cuthbert, “COVID was the straw that broke the camel’s back” on top of years of financial struggle (Pearl and Aldridge 2020). The closure meant that Culbert residents now had to drive 30 minutes to Eufaula, Alabama, or nearly an hour east to Albany, Georgia. There is only one ambulance to serve residents of Randolph County. In the segregated town of Cuthbert, many Black residents cannot afford to own a car and depend on the sole ambulance to transport them the long distance to a hospital. Randolph became the 55th county in the state without a hospital, and the first to see a hospital close during the pandemic (Barone 2020).
Phoebe Putney Health System said it was unable to come up with a plan to obtain the $10 million that Southwest Georgia Regional Medical Center needed for upgrades and renovations (Goldhill 2021). Given that the amount of CARES Act relief hospitals received from the Phase one general distribution fund was determined by their share of Medicare recipients and patient revenue, Southwest Georgia Regional Medical Center was disadvantaged because 54.5 percent of Cuthbert residents are on Medicaid and 11 percent are uninsured (Data USA 2021). The town was left with no alternative but to close its hospital’s doors. Given that Phoebe Putney Health System had funneled COVID-19 patients out of the hospital at the onset of the pandemic, the hospital also didn’t qualify for the later rounds of high-impact COVID-case dependent funds.
Two and a half hours north of Cubert is the 460-bed safety net hospital, Wellstar Atlanta Medical Center, in the large metropolis of Atlanta, which closed its doors a year and a half into the pandemic. Wellstar Health System, a state-wide chain, shut down its Atlanta Medical Center in November 2022. Wellstar is a nonprofit chain but that doesn’t mean they weren’t driven by the pursuit of profit when COVID-19 hit.
The hospital had served the historically Black Old Fourth Ward since 1901 and disproportionately provided services for low-income residents. Uncompensated care as a percent of operating expenses exceeded 16 percent from 2017-2021 which is far above the average acute care hospital’s 3 percent (Kacik 2022). Roughly two-thirds of its patient mix was Medicare, Medicaid, the uninsured, and indigent patients.
Wellstar Atlanta received $12,759,475 in federal relief in September 2020 from the High-Impact Payment program of the Provider Relief Fund (PRF) intended for safety net hospitals (HRSA 2021). Then in August 2021, it received a General Distribution Provider Relief Fund payment of $57,332,684 (HRSA 2024). In total, this is about $70 million.
Given the nature of the PRF formulas, Wellstar didn’t receive as much relief as its counterparts in Atlanta with higher patient revenue from private insurance. A hospital of a comparable size just twelve miles south in a wealthier part of the metro area, Northside Hospital Atlanta, received three times the CARES Act relief that Wellstar did.12 The relief came in two high-impact fund payments ($15,465,242 and $10,493,834.24) that followed an initial Phase one CARES Act General Distribution PRF payment of $204,289,212. In total that is roughly $230 million dollars, more than three times the $70 million Wellstar received. Table 2 (above) displays the ratio of hospital beds to COVID-19 stimulus received. Northside Hospital received $370,770 per patient bed compared to Wellstar Atlanta which received $152,374 per patient bed and Southwest Regional Medical Center which received $22,162 per patient bed.
Since Wellstar closed the Atlanta Medical Center, nearby facilities have been stretched to absorb the patient flow and the Black community served by the hospital has been left without a hospital in their neighborhood (Harris and McCorvey 2024).
Chicago’s two-tier health system illustrates the stark contrast between the allocation of CARES Act funds to safety net hospitals and to hospitals in university systems. In the initial round of high-impact payments, Northwestern Memorial Hospital received $35 million (HRSA 2024); in Phase 1 of General Distribution, it had received hundreds of millions to reimburse for lost Medicare fee-for-service revenue. At the same time, Chicago’s Loretto Hospital and Roseland Community Hospital both failed to meet the criteria for the first round of high-impact assistance (Terhune 2020). With a requirement of 100 inpatients treated for COVID-19 symptoms, Loretto missed the cutoff by a mere 15 patients (Goldberg 2020).
Loretto and Roseland are both located in Chicago’s low-income West and South Sides, respectively, while Northwestern Memorial Hospital serves communities north of the Chicago River, a generally affluent area.
The second round of high-impact funding in July 2020 gave some assistance to safety net hospitals, but the cash flow to university hospitals continued apace. Despite the fact that hospitals like Northwestern Memorial had access to vastly more reserves than safety net hospitals did, Northwestern received another $31 million in the second round of high-impact payments (HRSA 2021). When the number of patient beds are taken into account (Table 2 above), Northwestern Memorial Hospital received $386,497 per patient bed while Roseland Community Hospital received $111,614 and Loretto Hospital received $107,510 per patient bed.
The disproportionate burden on Chicago’s safety net hospitals became apparent during Thanksgiving week 2020, as intensive care beds filled up across many South Side hospitals that served primarily low-income Medicaid patients. At the same time, hundreds of ICU beds remained empty at the large university hospitals like Northwestern (Schorsch & Woelfel 2020). At Roseland Community Hospital, the emergency department was partially converted into inpatient beds to expand capacity. Specific information about availability of beds was “closely guarded” to manage capacity concerns. Though it was possible to transfer patients from the overburdened hospitals to the teaching hospitals with open beds, the hospitals with open beds can and did refuse the transfer. This system is patchwork and unreliable (Schorsch 2020).
The adverse situation these safety net hospitals face eventually led to labor unrest when workers at Loretto voted to authorize a strike in July 2023. Striking workers cited low pay and poor staffing conditions as reasons for the move (Davis 2023). Among the demands were $19/hour starting wages for certified nursing assistants, $17/hour starting wages for housekeepers, and more competitive remuneration across the board to help combat chronic understaffing. The strike was resolved after a few weeks, though the financial situation of the hospital continues to look dire (Liederman 2023).
This report has focused on a little-recognized and studied source of unequal patient care and health outcomes due to the uneven investment by hospitals in capital projects for new construction and renovation of hospital structures and for the acquisition of modern equipment and technology. The Hospital Survey and Construction Act of 1946 –the “Hill-Burton Act,” provided funding for the construction of nonprofit hospitals. The program was designed to remedy shortages of hospital capacity in poor and rural communities. Under its auspices, there were 5,567 capital projects focused on short-term general hospitals. Hill-Burton’s dark underbelly is that it wrote the racist views and patterns of segregation into its provisions, funding separate facilities for Black and white patients. Although this practice was halted in 1964, the long arm of racial injustice persists to the current day: nearly half of Black patients are cared for in just a small number of highly segregated hospitals.
Hill-Burton largely ended with the passage of Medicare in 1965 although it was phased out slowly. Since 1965, hospitals have mainly depended on their ability to generate internal funds for capital investment or on their ability to qualify for external funds borrowed in financial markets. For nonprofit hospitals, this consists mainly of issuing tax-free municipal bonds. In the first decades following the passage of Medicare, hospitals’ capital investments were subsidized by the federal government. The formulas for the subsidies disadvantaged smaller hospitals and those serving poor communities. These subsidies ended more than three decades ago.
This report examined how unequal access to financing has led to uneven quality of hospitals’ physical infrastructure and inequities in the care of patients. The COVID-19 pandemic revealed stark differences in the quality of care, with sometimes tragic consequences for Black COVID-19 patients. One study found that had Black patients been distributed among hospitals in the same proportions as white patients, the death rate of Black patients would have been reduced by 12 percent. Rural hospitals, with their older, poorer, and sicker patients and thin operating margins often have greater difficulties raising internal funds or borrowing in financial markets to replace and upgrade aging structures and out-of-date technology.
During the COVID-19 pandemic, Congress passed legislation to fund hospitals to care for the influx of patients. Surprisingly, these taxpayer dollars were allocated in a way that exacerbated the gap in quality of care among hospitals. Those treating Medicaid patients or the uninsured were largely excluded from the first and largest tranche of money distributed for such things as the purchase of ventilators, oxygen, remote monitoring equipment, PPE, and other safety equipment.
Hospitals with aging infrastructure that are most in need of upgrades often face the greatest challenges in accessing financing for capital investments. This is especially true of rural hospitals and those serving low-income Black, Indigenous, and immigrant communities. Hospitals in rural and other areas where deterioration of physical facilities that are on a downward trajectory and may not survive are other candidates for public financing of capital projects. The US needs to rethink the way hospitals finance the construction and modernization of health care facilities. The first step might be a targeted Hill-Burton Act for the 21st century that focuses on new construction, renovation, and modernization of hospitals in communities where it is most needed. Taxing profits above a threshold of for-profit subsidiaries of nonprofit hospitals could subsidize such an initiative.
It’s time to recognize that the quality of hospitals’ physical infrastructure affects patient safety and health outcomes, and for policymakers to develop targeted policies to address existing inequities in funding for capital projects.
Abelson, Reed. 2020. “HCA Reports Higher Earnings, Buffered by Millions in Coronavirus Relief.” The New York Times, July 22, 2020. https://www.nytimes.com/2020/07/22/business/hca-reports-higher-earnings-buffered-by-millions-in-coronavirus-relief.html.
Abramson, Alana. 2020. “Why the $2.2 Trillion-Dollar Bailout Benefited the Rich.” TIME, June 18, 2020, sec. Politics. https://time.com/5845116/coronavirus-bailout-rich-richer/.
Acosta, David A., and Sergio Aguilar-Gaxiola. 2014. “Academic Health Centers and Care of Undocumented Immigrants in the United States: Servant Leaders or Uncourageous Followers?” Academic Medicine 89 (4): 540–43. https://doi.org/10.1097/ACM.0000000000000182.
Akinleye, Dean D., Louise-Anne McNutt, Victoria Lazariu, and Colleen C. McLaughlin. 2019. “Correlation between Hospital Finances and Quality and Safety of Patient Care.” PLoS ONE 14 (8): e0219124. https://doi.org/10.1371/journal.pone.0219124.
Allard, Sam. 2024. “Cleveland Clinic Is Still among Nation’s Worst Hospitals for Community Spending.” Axios, April 2, 2024. https://www.axios.com/local/cleveland/2024/04/02/cleveland-clinic-fair-share-deficit-lown-institute-tax-breaks.
American Economic Liberties Project. 2023. “Critical Condition: How UPMC’s Monopoly Power Harms Workers and Patients.” American Economic Liberties Project. https://www.economicliberties.us/our-work/critical-condition-how-upmcs-monopoly-power-harms-workers-and-patients/.
American Hospital Association. 5/21. “Fact Sheet: Federal Investment Needed to Keep Hospitals’ Physical Infrastructure Ready to Meet the Nation’s Health Care Needs.” https://www.aha.org/system/files/media/file/2021/05/fact-sheet-physical-infrastructure-0521.pdf.
“Apollo’s Stranglehold on Hospitals Harms Patients and Healthcare Workers.” 2024. Private Equity Stakeholder Project. https://pestakeholder.org/wp-content/uploads/2024/01/PESP__Report_Apollo_Lifepoint_2024.pdf.
Appelbaum, Eileen, and Rosemary Batt. 2014. Private Equity at Work: When Wall Street Manages Main Street. Russell Sage Foundation.
———. 2016. “Fees, Fees and More Fees: How Private Equity Abuses Its Limited Partners and U.S. Taxpayers.” Center for Economic and Policy Research. https://cepr.net/report/private-equity-fees-2016-05/.
———. 2020. “Private Equity Buyouts in Healthcare: Who Wins, Who Loses?” Institute for New Economic Thinking. https://www.ineteconomics.org/research/research-papers/private-equity-buyouts-in-healthcare-who-wins-who-loses.
———. 2021. “Financialization in Health Care: The Transformation of US Hospital Systems.” Center for Economic and Policy Research.
Appelbaum, Eileen, Rosemary Batt, and Emma Curchin. 2023a. “Preying on the Dying: Private Equity Gets Rich in Hospice Care.” The Center for Economic and Policy Research. https://cepr.net/report/preying-on-the-dying-private-equity-gets-rich-in-hospice-care/.
———. 2023b. “Profiting at the Expense of Seniors: The Financialization of Home Health Care.” Center for Economic and Policy Research. https://cepr.net/report/profiting-at-the-expense-of-seniors-the-financialization-of-home-health-care/.
Asch, David A., Md Nazmul Islam, Natalie E. Sheils, Yong Chen, Jalpa A. Doshi, John Buresh, and Rachel M. Werner. 2021. “Patient and Hospital Factors Associated With Differences in Mortality Rates Among Black and White US Medicare Beneficiaries Hospitalized With COVID-19 Infection.” JAMA Network Open 4 (6): e2112842. https://doi.org/10.1001/jamanetworkopen.2021.12842.
Bah, Mamie. 2024. “State Lawmaker Questions Closing of UPMC’s Montefiore Dental Center – CBS Pittsburgh.” KDKA News, March 14, 2024. https://www.cbsnews.com/pittsburgh/news/state-lawmaker-question-closing-of-upmc-montefiore-dental-center/.
Bai, Ge, Farah Yehia, Wei Chen, and Gerard F. Anderson. 2020. “Varying Trends In The Financial Viability Of US Rural Hospitals, 2011–17.” Health Affairs 39 (6): 942–48. https://doi.org/10.1377/hlthaff.2019.01545.
Bailey, Brad. 2023. “COVID-19 Deaths Sped the Closure of Randolph County’s Only Hospital. What Happens Now?” Georgia Public Broadcasting, June 7, 2023. https://www.gpb.org/news/2023/06/07/covid-19-deaths-sped-the-closure-of-randolph-countys-only-hospital-what-happens-now.
Baker, Dean. 2024. “Declining Healthcare Costs: The Good Economic News Keeps Getting Better.” Center for Economic and Policy Research (blog). January 26, 2024. https://www.cepr.net/declining-healthcare-costs-the-good-economic-news-keeps-getting-better/.
Balasubramanian, Sai. 2023. “VCs Are Becoming Hyper-Focused On A Multibillion Dollar Opportunity: Healthcare Data.” Forbes, December 29, 2023, sec. Healthcare. https://www.forbes.com/sites/saibala/2023/12/29/vcs-are-becoming-hyper-focused-on-a-multibillion-dollar-opportunity-healthcare-data/.
Bannow, Tara. 2019. “Health Systems Consider Returning to Financing Derivatives as a Result of 2017 Tax Law.” Modern Healthcare, March 14, 2019, sec. Finance. https://www.modernhealthcare.com/finance/health-systems-consider-financing-derivatives-due-tax-law.
Barone, Emily. 2020. “Rural U.S. Hospitals Are on Life Support as a Third Wave of COVID-19 Strikes.” TIME, October 20, 2020. https://time.com/5901656/coronavirus-hospital-closures/.
Barrett, Mark. 2019. “Mission-HCA Deal Gets Key Regulatory OK from State Attorney General Stein.” The Asheville Citizen Times, January 16, 2019. https://www.citizen-times.com/story/news/local/2019/01/16/mission-health-asheville-josh-stein-hca-deal-can-go-forward-changes/2591769002/.
Basu, Sanjay, Seth A. Berkowitz, Caitlin Davis, Connor Drake, Robert L. Phillips, and Bruce E. Landon. 2023. “Estimated Costs of Intervening in Health-Related Social Needs Detected in Primary Care.” JAMA Internal Medicine 183 (8): 762–74. https://doi.org/10.1001/jamainternmed.2023.1964.
Batt, Rosemary, Eileen Applebaum, and Quynh Nguyen. 2023. “Pocketing Money Meant for Special Needs Kids: Private Equity in Autism Services.” Center for Economic and Policy Research.
Bazzoli, Gloria J., Richard C. Lindrooth, Romana Hasnain-Wynia, and Jack Needleman. 2004. “The Balanced Budget Act of 1997 and U.S. Hospital Operations.” Inquiry: A Journal of Medical Care Organization, Provision and Financing 41 (4): 401–17. https://doi.org/10.5034/inquiryjrnl_41.4.401.
Beardsley, Edward H. 1990. A History of Neglect: Health Care for Blacks and Mill Workers in the Twentieth-Century South. Univ. of Tennessee Press.
Beaulieu, Nancy D., Andrew L. Hicks, and Michael E. Chernew. 2024. “Hospital Market Dynamics: Prices, Capital Expenditures and Hospital Withering.” Harvard University Unpublished Paper, Working Paper Series, Department of Health Care Policy, Harvard Medical School (June).
Berard, Yamil. n.d. “Struggling Rural Georgia Hospital Calls It Quits.” The Atlanta Journal-Constitution, sec. COVID-19.
Bovbjerg, Randall R, and Robert A Berenson. 2/15. “Certificates of Public Advantage: Can They Address Provider Market Power?” Washington, DC: Urban Institute. https://www.urban.org/sites/default/files/publication/42226/2000111-Certificates-of-Public-Advantage.pdf.
Brecher, C., and S. Nesbitt. 1985. “Factors Associated with Variation in Financial Condition among Voluntary Hospitals.” Health Services Research 20 (3): 267–300.
Brown, Erin C Fuse. 2019. “To Oversee or Not to Oversee? Lessons from the Repeal of North Carolina’s Certificate of Public Advantage Law.” NY, NY: Milbank Memorial Fund.
Bruch, Joseph D., and David Bellamy. 2021. “Charity Care: Do Nonprofit Hospitals Give More than For-Profit Hospitals?” Journal of General Internal Medicine 36 (10): 3279–80. https://doi.org/10.1007/s11606-020-06147-9.
Burstin, H. R., S. R. Lipsitz, I. S. Udvarhelyi, and T. A. Brennan. 1993. “The Effect of Hospital Financial Characteristics on Quality of Care.” JAMA 270 (7): 845–49.
Cantor, Jonathan, Nabeel Qureshi, Brian Briscombe, Justin Chapman, and Christopher M. Whaley. 2021. “Association Between COVID-19 Relief Funds and Hospital Characteristics in the US.” JAMA Health Forum 2 (10): e213325. https://doi.org/10.1001/jamahealthforum.2021.3325.
“Capital Funding for Rural Healthcare.” 2024. Rural Health Information Hub. April 15, 2024. https://www.ruralhealthinfo.org/topics/capital-funding.
Carroll, Caitlin, Rhiannon Euhus, Nancy Beaulieu, and Michael E. Chernew. 2023. “Hospital Survival In Rural Markets: Closures, Mergers, And Profitability.” Health Affairs 42 (4): 498–507. https://doi.org/10.1377/hlthaff.2022.01191.
Cary, Peter. 2020. “Small and Rural Hospitals May Outlast COVID-19. But Can They Survive Trump’s Tax Law?” The Center for Public Integrity. http://publicintegrity.org/health/coronavirus-and-inequality/small-and-rural-hospitals-may-survive-covid-19-but-then-they-face-trumps-tax-law/.
Cass, Andrew. 2023. “Cleveland Clinic’s Payer Mix.” Becker’s Healthcare. December 1, 2023. https://www.beckershospitalreview.com/finance/cleveland-clinics-payer-mix.html.
Castele, Nick. 2020. “Mixed Feelings As Opportunity Corridor Nears Completion.” Ideastream Public Media, February 13, 2020, sec. Community. https://www.ideastream.org/community/2020-02-13/mixed-feelings-as-opportunity-corridor-nears-completion.
“Certificate of Public Advantage: Presentation to the House Select Committee on the Certificate of Need Process and Related Hospital Issues.” 2011. September 14. https://webservices.ncleg.gov/ViewDocSiteFile/43403.
Charles E. Cole Memorial Hospital d/b/a UPMC Cole. 2023. National Labor Relations Board.
Cheng, Kent Jason G, Yue Sun, and Shannon M Monnat. 2020. “COVID-19 Death Rates Are Higher in Rural Counties With Larger Shares of Blacks and Hispanics.” The Journal of Rural Health : Official Journal of the American Rural Health Association and the National Rural Health Care Association 36 (4): 602–8. https://doi.org/10.1111/jrh.12511.
Chung, Andrea Park, Martin Gaynor, and Seth Richards-Shubik. 2016. “Subsidies and Structure: The Lasting Impact of the Hill-Burton Program on the Hospital Industry.” Working Paper. Working Paper Series. National Bureau of Economic Research. https://doi.org/10.3386/w22037.
Clark, Lawrence J., Marilyn J. Field, Theodore L. Koontz, and Virginia L. Koontz. 1980. “The Impact of Hill-Burton: An Analysis of Hospital Bed and Physician Distribution in the United States, 1950-1970.” Medical Care 18 (5): 532–50. https://www.jstor.org/stable/3763902.
Cleveland Clinic Newsroom. 2022. “Cleveland Clinic Announces Details of $1.3 Billion in Capital Investments.” Cleveland Clinic. May 13, 2022. https://newsroom.clevelandclinic.org/2022/05/13/cleveland-clinic-announces-details-of-1-3-billion-in-capital-investments.
“Community Benefit State Law Profiles Comparison.” n.d. The Hilltop Institute. Accessed July 3, 2024. https://hilltopinstitute.org/our-work/hospital-community-benefit/hcbp-state-comparison/.
Conaway, Laura. 2009. “Struggling Braddock Loses Hospital, Economic Driver.” NPR, October 21, 2009, sec. Planet Money. https://www.npr.org/sections/money/2009/10/struggling_braddock_loses_hosp.html.
Cornely, Paul B. 1956. “Segregation and Discrimination in Medical Care in the United States.” American Journal of Public Health and the Nations Health 46 (9): 1074–81. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1624033/.
Coughlin, Teresa A. 08/22. “The COVID-19 Provider Relief Fund: Following How the US Department of Health and Human Services Distributed $178 Billion.” Urban Institute.
Czekalinski, Stephanie, and Michael Indriolo. 2022. “Cleveland Nonprofit Hospitals Get Millions in Property Tax Breaks. Many Are Asking, ‘Is It Worth It?’” Ideastream Public Media, June 21, 2022, sec. Government & Politics. https://www.ideastream.org/news/health-science/2022-06-21/cleveland-nonprofit-hospitals-get-millions-in-property-tax-breaks-many-are-asking-is-it-worth-it.
“Data USA: Cuthbert, GA.” 2021. Data USA (Data from the Census Bureau ACS 5-Year Estimate). 2021. https://datausa.io/profile/geo/cuthbert-ga.
Davis, Katherine. 2023. “Loretto Worker Strike Reverberates at Other Chicago Hospitals.” Crain’s Chicago Business, August 2, 2023, sec. Health Care. https://www.chicagobusiness.com/health-care/loretto-hospital-worker-strike-reverberates-other-chicago-hospitals.
DAVIS v. HCA HEALTHCARE, INC. Pending. North Carolina Judicial Branch.
Deto, Ryan. 2019. “Longtime UPMC Presbyterian Employee Spearheads Fight for Living Wage.” Pittsburgh City Paper, April 24, 2019. https://www.pghcitypaper.com/news/longtime-upmc-presbyterian-employee-spearheads-fight-for-living-wage-14823472.
———. n.d. “In Honor of UPMC CEO Romoff’s Retirement, a Look Back at His Loathsome Legacy.” Pittsburgh City Paper. Accessed April 30, 2024. https://www.pghcitypaper.com/news/in-honor-of-upmc-ceo-romoffs-retirement-a-look-back-at-his-loathsome-legacy-19915438.
Diamond, Dan. 2017. “How the Cleveland Clinic Grows Healthier While Its Neighbors Stay Sick.” POLITICO, July 17, 2017. http://www.politico.com/interactives/2017/obamacare-cleveland-clinic-non-profit-hospital-taxes/.
Diaz, Naomi. 2023. “23 Health Systems with Investment Arms.” September 7, 2023. https://www.beckershospitalreview.com/innovation/22-health-systems-with-investment-arms.html.
“Distribution of the Nonelderly with Medicaid by Race/Ethnicity.” 2022. KFF (blog). 2022. https://www.kff.org/medicaid/state-indicator/medicaid-distribution-nonelderly-by-raceethnicity/.
D’Silva, Adrian, Haley Gregg, and David Marshall. 2008. “Explaining the Decline in the Auction Rate Securities Market.” Federal Reserve Bank of Chicago, No. 256. https://www.chicagofed.org/publications/chicago-fed-letter/2008/november-256.
Duffy, S. Q., and B. Friedman. 1993. “Hospitals with Chronic Financial Losses: What Came Next?” Health Affairs (Project Hope) 12 (2): 151–63. https://doi.org/10.1377/hlthaff.12.2.151.
Dugan, Ianthe Jeanne. 2010. “Hospitals’ Wall Street Wounds.” The Wall Street Journal, July 7, 2010. https://www.wsj.com/articles/SB10001424052748704545004575353190698790172.
Eble, Jack. 2019. “UPMC Pinnacle Lancaster Hospital Officially Closes, Services Transitioned to UPMC Pinnacle Lititz.” Fox43, February 28, 2019. https://www.fox43.com/article/news/local/contests/upmc-pinnacle-lancaster-hospital-officially-closes-services-transitioned-to-upmc-pinnacle-lititz/521-23165865-3ea8-4e0d-88eb-1e471e91b743.
Ellison, Ayla. 2020. “HHS Unveils Plan to Deliver $40B in COVID-19 Aid to Hospitals.” Becker’s Hospital Review, April 23, 2020. https://www.beckershospitalreview.com/finance/hhs-unveils-plan-to-deliver-40b-in-covid-19-aid-to-hospitals.html.
Enumah, Samuel J., and David C. Chang. 2021. “Predictors of Financial Distress Among Private U.S. Hospitals.” Journal of Surgical Research 267 (November):251–59. https://doi.org/10.1016/j.jss.2021.05.025.
Epané, Josué Patien, Ferhat Zengul, Zo Ramamonjiarivelo, Luceta McRoy, and Robert Weech-Maldonado. 2023. “Resources Availability and COVID-19 Mortality among US Counties.” Frontiers in Public Health 11 (March):1098571. https://doi.org/10.3389/fpubh.2023.1098571.
Evans, Melanie. 2010. “Risk and Reward.” Modern Healthcare, June 18, 2010, sec. Finance. https://www.modernhealthcare.com/article/20100621/MAGAZINE/100619921/risk-and-reward.
Exemptions Related to Access to Hospital and Health Care Services by Low-Income and Underserved Individuals. 2012. Property Tax Code. Vol. Section 35 ILCS 200/15-86. https://casetext.com/statute/illinois-compiled-statutes/government/chapter-35-revenue/subchapter-property-taxes/act-200-property-tax-code/article-15-exemptions/section-35-ilcs-20015-86-exemptions-related-to-access-to-hospital-and-health-care-services-by-low-income-and-underserved-individuals.
Felton, Julia. 2024. “Pittsburgh Targets More Tax-Exempt Properties, Including 61 Owned by UPMC.” TribLIVE.Com, March 27, 2024, sec. Local. https://triblive.com/local/pittsburgh-challenging-tax-exempt-status-of-104-properties-more-than-half-owned-by-upmc/.
Fox, D. M., and D. C. Schaffer. 1991. “Tax Administration as Health Policy: Hospitals, the Internal Revenue Service, and the Courts.” Journal of Health Politics, Policy and Law 16 (2): 251–79. https://doi.org/10.1215/03616878-16-2-251.
Franklin, John. 2020. “What Are ‘Cinderella Bonds’?” Pearl Creek Advisors, LLC, Comprehensive Capital Reforms Advice, September. https://static1.squarespace.com/static/5e1a0c58bf964c7a9a9ab0d8/t/5f748407e5310349ea4bc240/1601471502549/PCA-Paper.CinderellaBonds.pdf.
Gabriel, Meghan Hufstader, Chelsea Richwine, Catherine Strawley, Wesley Barker, and Jordan Everson. 2024. “Interoperable Exchange of Patient Health Information Among U.S. Hospitals: 2023.” ONC Data Brief, No. 71. Office of the National Coordinator for Health Technology. https://www.healthit.gov/sites/default/files/2024-05/Interoperable-Exchange-of-Patient-Health-Information-Among-U.S.-Hospitals-2023.pdf.
Gee, Emily, and Thomas Waldrop. 2022. “Policies To Hold Nonprofit Hospitals Accountable.” Center for American Progress. https://www.americanprogress.org/article/policies-to-hold-nonprofit-hospitals-accountable/.
Georgia Public Broadcasting, dir. 2023. The Citizens of Cuthbert, Georgia Grapple with the Loss of the Town’s Only Hospital. https://www.youtube.com/watch?v=SB-iK9KIRn4.
Godwin, Jamie, Zachary Levinson, and Scott Hulver. 2023. “The Estimated Value of Tax Exemption for Nonprofit Hospitals Was About $28 Billion in 2020.” Kaiser Family Foundation. https://www.kff.org/health-costs/issue-brief/the-estimated-value-of-tax-exemption-for-nonprofit-hospitals-was-about-28-billion-in-2020/.
Goldberg, Stephanie. 2020. “Why Some Smaller Hospitals Treating Lots of COVID Patients Aren’t Getting ‘high-Impact’ Federal Aid.” Modern Healthcare. June 1, 2020. https://www.modernhealthcare.com/finance/some-smaller-hospitals-miss-out-covid-federal-aid.
Goldhill, Olivia. 2021. “Shuttered Hospitals, Soaring Covid-19 Deaths: Rural Black Communities Lose a Lifeline in the Century’s Worst Health Crisis.” STAT, May 26, 2021. https://www.statnews.com/2021/05/26/shuttered-hospitals-soaring-covid19-deaths-rural-black-communities-lose-lifeline-in-pandemic/.
Gondi, Suhas, and Zirui Song. 2019. “The Burgeoning Role Of Venture Capital In Health Care.” Health Affairs, January. https://doi.org/10.1377/forefront.20181218.956406.
Government Accountability Office. 2023. “Testimony Before the Subcommittee on Oversight, Committee on Ways and Means, House of Representatives: IRS Oversight of Hospitals’ Tax-Exempt Status.” GAO Publication No. 23-106777. Washington, DC. https://www.gao.gov/assets/gao-23-106777.pdf.
Greene, Jay. 2008. “Local Hospitals Flee Auction-Rate Bond Market.” Crain’s Detroit Business, May 1, 2008. https://www.crainsdetroit.com/article/20080501/EMAIL01/503584665/local-hospitals-flee-auction-rate-bond-market.
Grogan, Colleen M. 2023. Grow and Hide: The History of America’s Health Care State. Oxford, New York: Oxford University Press.
Grogan, Colleen M., Yu-An Lin, and Michael K. Gusmano. 2021. “Unsanitized and Unfair: How COVID-19 Bailout Funds Refuel Inequity in the US Health Care System.” Journal of Health Politics, Policy and Law 46 (5): 785–809. https://doi.org/10.1215/03616878-9155977.
Gu, Amy Y. 2019. “[Case Watch] Commonwealth of Pennsylvania v. UPMC and Highmark: State AG Prevails with 10-Year Consent Decree After Long Bitter Court Battle.” The Source on HealthCare Price and Competition. September 16, 2019. https://sourceonhealthcare.org/case-watch-commonwealth-of-pennsylvania-v-upmc-and-highmark-state-ag-prevails-with-10-year-consent-decree-after-long-bitter-court-battle/
Halleman, Sydney. 2023. “UPMC, Washington Ink Definitive Merger Agreement.” Healthcare Dive, October 25, 2023. https://www.healthcaredive.com/news/upmc-washington-definitive-merger-agreement/697744/.
Hamill, Sean. 2022. “Medical Debt Buries Some at UPMC.” Pittsburgh Post-Gazette, January 30, 2022. https://www.post-gazette.com/business/healthcare-business/2022/01/30/Pittsburgh-UPMC-workers-medical-debt/stories/202201300046.
Harris, Bracey, and J.J. McCorvey. 2024. “Atlanta’s Health Care System Is Strained by Major Hospital’s Closing, Doctors and Patients Say.” NBC News, February 7, 2024. https://www.nbcnews.com/news/us-news/hospitals-strained-atlanta-medical-center-closing-doctors-rcna137451.
Hawryluk, Markian. 2024. “Rural Hospitals Face Aging Infrastructure amid Financial Hurdles.” Modern Healthcare, January 12, 2024, sec. Providers. https://www.modernhealthcare.com/providers/rural-hospitals-aging-infrastructure-financial-issues-capital-improvements.
Health Resources & Services Administration. 2021. “Provider Relief Fund COVID-19 High-Impact Payments.” https://data.cdc.gov/Administrative/Provider-Relief-Fund-COVID-19-High-Impact-Payments/b58h-s9zx/data_preview.
———. 2024. “HHS Provider Relief Fund.” https://data.cdc.gov/Administrative/HHS-Provider-Relief-Fund/kh8y-3es6/data_preview
Henderson, Jan. 2024. “Academic Medical Centers: Education or Profits?” The Health Culture. 2024. https://www.thehealthculture.com/2015/07/academic-medical-centers-education-or-profits/.
Heshmat, Shahram. 1992. “Estimating the Cost of Capital for Nonprofit Hospitals.” Journal of Health and Human Resources Administration 14 (4): 465–73. https://www.jstor.org/stable/25780511.
Hill, Latoya, and Samantha Artiga. 2022. “COVID-19 Cases and Deaths by Race/Ethnicity: Current Data and Changes Over Time.” Kaiser Family Foundation. https://www.kff.org/coronavirus-covid-19/issue-brief/covid-19-cases-and-deaths-by-race-ethnicity-current-data-and-changes-over-time/.
“Hill-Burton Act.” 2020. Harvard University Center for the History of Medicine at Countway Library. Perspectives Of Change (blog). 2020. https://perspectivesofchange.hms.harvard.edu/node/23.
Hoban, Rose. 2015. “Rural Hospital Bill Portends Larger Changes for N.C. Hospitals.” North Carolina Health News, November 6, 2015. http://www.northcarolinahealthnews.org/2015/11/06/rural-hospital-bill-portends-larger-changes-for-n-c-hospitals/.
Hollingsworth, Alex, Krzysztof Karbownik, Melissa A. Thomasson, and Anthony Wray. 2024. “The Gift of a Lifetime: The Hospital, Modern Medicine, and Mortality.” American Economic Review 114 (7): 2201–38. https://doi.org/10.1257/aer.20230008.
Hoyert, Donna L. 2021. “Maternal Mortality Rates in the United States, 2019.” National Center for Health Statistics. June 10, 2021. https://www.cdc.gov/nchs/data/hestat/maternal-mortality-2021/maternal-mortality-2021.htm.
Hudson, Caroline. 2024a. “Health Systems Invest in New Facilities, Services to Grow Revenue.” Modern Healthcare, January 8, 2024, sec. Finance. https://www.modernhealthcare.com/finance/sanford-health-upmc-capital-projects-revenue-growth.
———. 2024b. “UPMC Acquires Washington Health System June 1.” Modern Healthcare, June 3, 2024, sec. Mergers & Acquisitions. https://www.modernhealthcare.com/mergers-acquisitions/upmc-washington-health-system-merger-brook-ward.
Internal Revenue Service. 1998. “Rev. Rul. 98-15, 1998-12 I.R.B.” https://www.irs.gov/pub/irs-drop/rr-98-15.pdf.
———. n.d. “Understanding IRS Guidance – A Brief Primer | Internal Revenue Service.” Accessed June 10, 2024. https://www.irs.gov/newsroom/understanding-irs-guidance-a-brief-primer.
IRS (Internal Revenue Service). 1956. “Rev. Rul. 56-185, 1956-1 C.B. 202.” https://www.irs.gov/pub/irs-tege/rr69-545.pdf.
———. 1969. “C.B. 117. Revenue Ruling 69-545.” https://www.irs.gov/pub/irs-tege/rr69-545.pdf.
———. 2023. “Schedule H (Form 990): Hospitals.” Internal Revenue Service. 2023. https://www.irs.gov/instructions/i990sh.
Janke, Alexander T, Hao Mei, Craig Rothenberg, Robert D Becher, Zhenqiu Lin, and Arjun K Venkatesh. 2021. “Analysis of Hospital Resource Availability and COVID-19 Mortality Across the United States.” Journal of Hospital Medicine 16 (4): 211–14. https://doi.org/10.12788/jhm.3539.
Jeurissen, Patrick P. T., Florien M. Kruse, Reinhard Busse, David U. Himmelstein, Elias Mossialos, and Steffie Woolhandler. 2021. “For-Profit Hospitals Have Thrived Because of Generous Public Reimbursement Schemes, Not Greater Efficiency: A Multi-Country Case Study.” International Journal of Health Services 51 (1): 67–89. https://doi.org/10.1177/0020731420966976.
Jha, Ashish K., E. John Orav, Zhonghe Li, and Arnold M. Epstein. 2007a. “Concentration and Quality of Hospitals That Care for Elderly Black Patients.” Archives of Internal Medicine 167 (11): 1177–82. https://doi.org/10.1001/archinte.167.11.1177.
John, Randall, Tyler Malone, and George Pink. 2022. “Trends in Revenue Sources among Rural Hospitals.” UNC Sheps Center: NC Rural Health Research Program.
Kacik, Alex. 2020. “Top Not-for-Profit Hospitals Offer Disproportionately Less Charity Care, Study Finds.” Modern Healthcare, February 18, 2020, sec. Providers. https://www.modernhealthcare.com/providers/charity-care-markedly-lower-richest-not-profit-hospitals.
———. 2022. “Wellstar Health System to Close Atlanta Medical Center.” Modern Healthcare, September 1, 2022, sec. Providers. https://www.modernhealthcare.com/providers/wellstar-health-system-close-atlanta-medical-center.
Kibler, William. 2023. “NLRB: UPMC Altoona Violated Federal Law.” Atlanta Mirror, March 11, 2023. https://www.altoonamirror.com/news/local-news/2023/03/nlrb-upmc-altoona-violated-federal-law/.
Kim, Tae Hyun, and Michael J. McCue. 2008. “Association of Market, Operational, and Financial Factors with Nonprofit Hospitals’ Capital Investment.” INQUIRY: The Journal of Health Care Organization, Provision, and Financing 45 (2): 215–31. https://doi.org/10.5034/inquiryjrnl_45.02.215.
Largent, Emily A. 2018. “Public Health, Racism, and the Lasting Impact of Hospital Segregation.” Public Health Reports 133 (6): 715–20. https://doi.org/10.1177/0033354918795891.
Lasser, Karen E., Zhixiu Liu, Meng-Yun Lin, Michael K. Paasche-Orlow, and Amresh Hanchate. 2021. “Changes in Hospitalizations at US Safety-Net Hospitals Following Medicaid Expansion.” JAMA Network Open 4 (6): e2114343. https://doi.org/10.1001/jamanetworkopen.2021.14343.
Lave, Judith R., and Lester B. Lave. 1974. The Hospital Construction Act: An Evaluation of the Hill-Burton Program, 1948-1973. Evaluative Studies, 16. Washington: American Enterprise Institute for Public Policy Research.
Levey, Noam N. 2022. “Few Places Have More Medical Debt Than Dallas-Fort Worth, but Hospitals There Are Thriving.” KFF Health News, September 28, 2022. https://kffhealthnews.org/news/article/medical-debt-hospitals-dallas-fort-worth/.
Liederman, Mack. 2023. “Loretto Hospital Strike Ends As Workers Claim ‘Victory’ With Tentative Contract.” Block Club Chicago, August 11, 2023. http://blockclubchicago.org/2023/08/11/loretto-hospital-strike-ends-as-workers-claim-victory-with-tentative-contract/.
Liss, Samantha. 2019. “Investment Income Plays Important Role for Nonprofit Hospitals, Fitch Says.” Healthcare Dive, October 17, 2019. https://www.healthcaredive.com/news/investment-income-plays-important-role-for-nonprofit-hospitals-fitch-says/565223/.
———. 2020. “For-Profit, Higher-Margin Hospitals at Advantage When It Comes to CARES Funding.” Healthcare Dive, May 14, 2020. https://www.healthcaredive.com/news/for-profit-higher-margin-hospitals-at-advantage-when-it-comes-to-cares-fun/577941/.
Lopez, Eric, Tricia Neuman, Gretchen Jacobson, and Larry Levitt. 2020. “How Much More Than Medicare Do Private Insurers Pay? A Review of the Literature.” KFF. https://www.kff.org/medicare/issue-brief/how-much-more-than-medicare-do-private-insurers-pay-a-review-of-the-literature/.
Marcetic, Branko. 2018. “The Hospital That Held a City Hostage.” Jacobin, September 30, 2018. https://jacobin.com/2018/09/pittsburgh-upmc-hospital-single-payer-amazon.
Mathews, Anna Wilde, Tom McGinty, and Melanie Evans. 2022. “Big Hospitals Provide Skimpy Charity Care—Despite Billions in Tax Breaks.” Wall Street Journal, July 25, 2022, sec. Business. https://www.wsj.com/articles/nonprofit-hospitals-vs-for-profit-charity-care-spending-11657936777.
Mayes, Rick, and Robert A. Berenson. 2006. Medicare Prospective Payment and the Shaping of U.S. Health Care. John Hopkins University Press.
McDaniels, Andrea K. 2013. “UMMS Defends Use of Interest Rate Swaps.” The Baltimore Sun, September 13, 2013. https://www.baltimoresun.com/2013/09/13/umms-defends-use-of-interest-rate-swaps/.
Meltsner, Michael. 1966a. “Equality and Health.” SSRN Scholarly Paper. Rochester, NY. https://papers.ssrn.com/abstract=2065942.
———. 1966b. “Equality and Health.” SSRN Scholarly Paper. Rochester, NY. https://papers.ssrn.com/abstract=2065942.
Miller, Andy, and Markian Hawryluk. 2023a. “As Nonprofit Hospitals Reap Big Tax Breaks, States Scrutinize Their Required Charity Spending.” KFF Health News, July 11, 2023. https://kffhealthnews.org/news/article/nonprofit-hospitals-tax-breaks-community-benefit/.
———. 2023b. “Nonprofit Hospitals under Growing Scrutiny over How They Justify Billions in Tax Breaks.” CNN, July 10, 2023. https://www.cnn.com/2023/07/10/health/nonprofit-hospitals-community-benefits-kff-health-news/index.html.
Miller, Brenna. 2024. “2024 Fair Share Spending: Top 10 Systems.” Lown Institute. https://lowninstitute.org/2024-fair-share-spending-top-10-systems/.
Minemyer, Paige. 2017. “UPMC Will Invest $2B to Build 3 Specialty Hospitals.” Fierce Healthcare, November 6, 2017. https://www.fiercehealthcare.com/finance/upmc-capital-investment-allegheny-health-network-hospital-expansion.
More Perfect Union, dir. 2023. The Greediest “Non-Profit” Hospital in America. https://www.youtube.com/watch?v=3tK_UHD1pD8.
Morgenson, Gretchen. 2024a. “Cancer Patients Say This Hospital Denied Them Care.” NBC News, June 5, 2024. https://www.nbcnews.com/health/cancer/cancer-patients-say-new-mexico-hospital-turned-them-away-rcna147184.
———. 2024b. “The States Where Private Equity Has the Most Sway over Housing, Health Care, Jobs and Pensions.” NBC News. April 9, 2024. https://www.nbcnews.com/news/us-news/states-rank-private-equity-influence-housing-health-care-jobs-pensions-rcna146818.
Mouch, Charles A., Scott E. Regenbogen, Sha’Shonda L. Revels, Sandra L. Wong, Christy H. Lemak, and Arden M. Morris. 2014. “The Quality of Surgical Care in Safety Net Hospitals: A Systematic Review.” Surgery 155 (5): 826–38. https://doi.org/10.1016/j.surg.2013.12.006.
Moura, Paula. 2021. “What Is a Safety-Net Hospital and Why Is It So Hard to Define?” FRONTLINE, May 18, 2021. https://www.pbs.org/wgbh/frontline/article/what-is-a-safety-net-hospital-covid-19/.
Muoio, Dave. 2023. “Unions Ask DOJ to Investigate UPMC for Worker Suppression.” Fierce Healthcare, May 18, 2023, sec. Fierce Healthcare Homepage, Payers, Hospitals, Regulatory. https://www.fiercehealthcare.com/providers/unions-ask-doj-investigate-upmc-alleged-anticompetitive-worker-suppression.
Ndugga, Nambi, Latoya Hill, and Samantha Artiga. 2024. “Introduction – Key Data on Health and Health Care by Race and Ethnicity | KFF.” Kaiser Family Foundation. https://www.kff.org/key-data-on-health-and-health-care-by-race-and-ethnicity/?entry=executive-summary-introduction.
Nixdorf, Katie, and Josh Hirschfeld-Kroen. 2023. “UPMC: The Greediest ‘Non-Profit’ Hospital in America.” More Perfect Union, July 14, 2023. https://perfectunion.us/greediest-hospital-upmc/.
“Nonprofit Hospitals Receive Billions More in Tax Breaks than They Invest in Their Communities.” n.d. Lown Institute Hospital Index (blog). Accessed April 22, 2024. https://lownhospitalsindex.org/2023-fair-share-spending/.
O’Grady, Eileen, Mary Bugbee, and Michael Fenne. 2023. “Private Equity Descends on Rural Healthcare.” Private Equity Stakeholder Project. https://pestakeholder.org/wp-content/uploads/2023/02/PE_Rural_Health_Jan2023-compressed.pdf.
Olsen, Emily. 2023. “CMS Launches Primary Care Pilot to Expand Value-Based Care.” Healthcare Dive, June 9, 2023. https://www.healthcaredive.com/news/CMS-launches-Making-Care-Primary-value-based-care-model/652491/.
Owermohle, Sarah. 2023. “Senators Push IRS to Launch Nonprofit Hospital Probe.” STAT News, August 8, 2023. https://www.statnews.com/2023/08/08/senators-nonprofit-hospital-probe/.
Pearl, Matt, and Donesha Aldridge. 2020. “Evictions, Poverty, and Underserved Communities | The Ripple Effects of COVID-19 in Georgia.” 11Alive News, October 23, 2020, sec. 11alive, news, health, coronavirus, local. https://www.11alive.com/article/news/health/coronavirus/the-ripple-effects-of-covid-19-in-georgia/85-26c7290a-d2ef-4d0c-9aea-8d070c1f85ca.
Pennsylvania General Assembly. 1997. Institutions of Purely Public Charity Act. 1997 Act 55. Vol. P.L. 508. https://www.legis.state.pa.us/cfdocs/Legis/LI/uconsCheck.cfm?txtType=HTM&yr=1997&sessInd=0&smthLwInd=0&act=0055.
Phillips, Lauren. 2013. “How to Take Advantage of HUD’s Hospital Mortgage Insurance Program,” Healthcare Financial Management Association Newsletter, May. https://www.hud.gov/sites/documents/OHF_HFMA_ARTICLE.PDF.
Pifer, Rebecca. 2020. “In Surprise Move, HCA to Return All $6B in COVID-19 Federal Aid.” Healthcare Dive, October 9, 2020. https://www.healthcaredive.com/news/in-surprise-move-hca-to-return-all-6b-in-covid-19-federal-aid/586736/.
———. 2022. “Hospitals Bet Big on Venture Capital amid COVID-19 Revenue Flux.” Healthcare Dive, March 30, 2022. https://www.healthcaredive.com/news/hospital-venture-capital-COVID-19/619852/.
———. 2023. “CMS Exploring Models Centered on Social Health Factors.” Healthcare Dive, June 9, 2023. https://www.healthcaredive.com/news/cms-social-determinants-health-equity-medicare/652571/.
Pitchbook Cleveland Clinic Innovations. 2024. Pitchbook Cleveland Clinic Innovations Profile, as of July 8, 2024. Downloaded July 8, 2024.
“Policies To Hold Nonprofit Hospitals Accountable.” 2022. Center for American Progress (blog). October 18, 2022. https://www.americanprogress.org/article/policies-to-hold-nonprofit-hospitals-accountable/.
Pozner, Robert S. 2015. “Asheville’s Growth Began with 19th Century TB Treatment.” The Asheville Citizen Times, July 20, 2015. https://www.citizen-times.com/story/life/2015/07/20/ashevilles-growth-began-th-century-tb-treatment/30408281/.
Radley, David C., Arnav Shah, Sara R. Collins, Neil R. Powe, and Laurie Zephyrin. 2024. “Advancing Racial Equity in U.S. Health Care: The Commonwealth Fund 2024 State Health Disparities Report.” The Commonwealth Fund. https://doi.org/10.26099/vw02-fa96.
Rau, Jordan. 2021. “Mission and Money Clash in Nonprofit Hospitals’ Venture Capital Ambitions.” KFF Health News, August 24, 2021. https://kffhealthnews.org/news/article/mission-and-money-clash-in-nonprofit-hospitals-venture-capital-ambitions/.
Rau, Jordan, and Emmarie Huetteman. 2020. “Some Urban Hospitals Face Closure Or Cutbacks As The Pandemic Adds To Fiscal Woes.” NPR, September 15, 2020, sec. Health Reporting in the States. https://www.npr.org/sections/health-shots/2020/09/15/912866179/some-urban-hospitals-face-closure-or-cutbacks-as-the-pandemic-adds-to-fiscal-woe.
Reynolds, P. Preston. 2004. “Professional and Hospital DISCRIMINATION and the US Court of Appeals Fourth Circuit 1956–1967.” American Journal of Public Health 94 (5): 710–20. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1448322/.
Richards, Catherine. 2014. “The Effect of Hospital Financial Distress on Immediate Breast Reconstruction.” Columbia University. https://doi.org/10.7916/D8C53HZ2.
Rose, Rachel V. 2012. “The Silver Lining for Non-Profit Hospitals: Utilizing Bond Derivative Swaps to Control Costs and Generate Revenue.” Becker’s Healthcare. September 7, 2012. https://www.beckershospitalreview.com/finance/the-silver-lining-for-non-profit-hospitals-utilizing-bond-derivative-swaps-to-control-costs-and-generate-revenue.html.
Ross, Janell. 2021. “The Massive Role That Medicare Played in Racial Integration.” Washington Post, November 25, 2021. https://www.washingtonpost.com/news/the-fix/wp/2015/07/31/the-massive-role-that-medicare-played-in-racial-integration/.
“Rural Hospitals – Funding & Opportunities.” n.d. Rural Health Information Hub. Accessed July 3, 2024. https://www.ruralhealthinfo.org/topics/hospitals/funding.
Sanders, Bernard. 2023. “Major Non-Profit Hospitals Take Advantage of Tax Breaks and Prioritize CEO Pay Over Helping Patients Afford Medical Care.” United States Senate: Health, Education, Labor, and Pensions Committee. https://www.sanders.senate.gov/wp-content/uploads/Executive-Charity-HELP-Committee-Majority-Staff-Report-Final.pdf.
Sarkar, Reith R., P. Travis Courtney, Katie Bachand, Paige E. Sheridan, Paul J. Riviere, Zachary D. Guss, Christian R. Lopez, Michael G. Brandel, Matthew P. Banegas, and James D. Murphy. 2020. “Quality of Care at Safety-Net Hospitals and the Impact on Pay-for-Performance Reimbursement.” Cancer 126 (20): 4584–92. https://doi.org/10.1002/cncr.33137.
Schafron, Sean. 2010. “Community Opposes Hospital Closing.” Workers World Pittsburgh. January 30, 2010. https://www.workers.org/2010/us/pittsburgh_0204/.
Schorsch, Kristen. 2020. “The Pandemic Revealed Another Gap In Chicago Health Care: Hospitals Are On Their Own To Transfer Patients.” WBEZ Chicago, June 29, 2020, sec. Environment & Public Health. https://www.wbez.org/stories/one-chicago-hospital-called-for-8-hours-to-transfer-covid-19-patients-thats-problematic-for-future-outbreaks/1ecd60f3-f185-4deb-ae65-3e3ca25f0063.
Schorsch, Kristen, and Mariah Woelfel. 2020. “When Some Small Hospitals In Chicago Were Full, Bigger Ones Had Beds To Spare.” WBEZ Chicago, December 9, 2020, sec. Coronavirus in Illinois. https://www.wbez.org/stories/when-some-small-hospitals-in-chicago-were-full-bigger-ones-had-beds-to-spare/c08f8b56-b637-48ac-809b-d5303243bf82.
Schumann, John Henning. 2016. “A Bygone Era: When Bipartisanship Led To Health Care Transformation.” NPR, October 2, 2016, sec. Public Health. https://www.npr.org/sections/health-shots/2016/10/02/495775518/a-bygone-era-when-bipartisanship-led-to-health-care-transformation.
Schwartz, Karyn, and Anthony Damico. 2020. “Distribution of CARES Act Funding Among Hospitals.” KFF (blog). May 13, 2020. https://www.kff.org/coronavirus-covid-19/issue-brief/distribution-of-cares-act-funding-among-hospitals/.
Schwartz, Karyn, Eric Lopez, Matthew Rae, and Tricia Neuman. 2020. “What We Know About Provider Consolidation.” KFF (blog). September 2, 2020. https://www.kff.org/health-costs/issue-brief/what-we-know-about-provider-consolidation/.
Scott, S.J. 1984. “The Medicare Prospective Payment System.” American Journal of Occupational Therapy 38(5): 330-334.
SEIU Healthcare Pennsylvania, and Strategic Organizing Center. 2023. “Complaint Against University of Pittsburgh Medical Center Regarding Potential Attempted and Actual Monopolization and Monopsonization In Violation of Section 2 of the Sherman Act.” https://thesoc.org/wp-content/uploads/2023/05/COMPLAINT_5.17_redacted.pdf.
Sen, Astha, Nicholas Warner, Meghna Paul, Jake Vaughan, and Peter Bluestone. 12/23. “Tax Incentive Evaluation: Non-Profit Hospital Exemptions.” Atlanta, Georgia: Georgia State University Fiscal Research Center. https://www.open.ga.gov/openga/report/downloadFile?rid=30420.
Shakoor, Aly, Emily Gee, and Nicole Rapfogel. 2020. “Health Care Providers in Georgia’s Low-Income Communities Need Financial Relief.” Center for American Progress, December 15, 2020. https://www.americanprogress.org/article/health-care-providers-georgias-low-income-communities-need-financial-relief/.
Sherlock, D. B. 1986. “Indigent Care in Rational Markets.” Inquiry: A Journal of Medical Care Organization, Provision and Financing 23 (3): 261–67.
Smith, D.B. 2016. The Power to Heal: Civil Rights, Medicare, and the Struggle to Transform America’s Health Care System. Vanderbilt University Press. https://books.google.com/books?id=f0CzDAAAQBAJ.
Stewart, Louis J., and Vincent Owhoso. 2004. “Derivative Financial Instruments and Nonprofit Health Care Providers.” Journal of Health Care Finance 31 (2): 38–52.
Stewart, Louis J., and Pamela C. Smith. 2012. “The 2008 Auction Rate Securities Market Collapse and US Nonprofit Health System.” Qualitative Research in Financial Markets 4(1): 68-83 (April).
Terhune, Chad. 2020. “Billions in COVID Relief Go to Biggest Hospital Chains as Smaller Rivals Await Aid.” Reuters, June 9, 2020. https://www.reuters.com/article/idUSKBN23G1GH/.
“The Hospital Survey and Construction Act.” 1946. Journal of the American Medical Association 132 (3): 148–49. https://doi.org/10.1001/jama.1946.02870380030010.
Thomas, Karen Kruse. 2006. “The Hill-Burton Act and Civil Rights: Expanding Hospital Care for Black Southerners, 1939-1960.” The Journal of Southern History 72 (4): 823–70. https://doi.org/10.2307/27649234.
———. 2008. “Hill-Burton Act.” Encyclopedia of Alabama. January 22, 2008. https://encyclopediaofalabama.org/article/hill-burton-act/.
Thomas, Sharita R, George H Pink, and G Mark Holmes. 2016. “Geographic Variation in the Profitability of Urban and Rural Hospitals.” NC Rural Health Research Program, University of North Carolina, March.
Tiel, Rebecca. 2019. “What Oregon’s New Hospital Charity Care Law Means for You.” Our Health Oregon. September 17, 2019. https://ourhealthoregon.org/news/what-oregons-new-hospital-charity-care-law-means-for-you.
Tikkanen, Roosa Sofia, Steffie Woolhandler, David U. Himmelstein, Nancy R. Kressin, Amresh Hanchate, Meng-Yun Lin, Danny McCormick, and Karen E. Lasser. 2017. “Hospital Payer and Racial/Ethnic Mix at Private Academic Medical Centers in Boston and New York City.” International Journal of Health Services : Planning, Administration, Evaluation 47 (3): 460–76. https://doi.org/10.1177/0020731416689549.
Tkacik, Maureen. 2023. “The Moral Authority of Marc Rowan.” The American Prospect, October 21, 2023. https://prospect.org/api/content/a42cec1e-6fab-11ee-9d32-12163087a831/.
Toleos, Aaron. 2024. “PRESS RELEASE: More than 1,900 Nonprofit Hospitals Receive More in Tax Breaks than They Give Back to Their Community, Totaling Billions.” Lown Institute (blog). March 26, 2024. https://lowninstitute.org/press-release-more-than-1900-nonprofit-hospitals-receive-more-in-tax-breaks-than-they-give-back-to-their-community-totaling-billions/.
“Top Hospitals in Georgia (GA) by Net Patient Revenue.” n.d. Accessed April 10, 2024. https://www.definitivehc.com/resources/healthcare-insights/top-hospitals-georgia-net-patient-revenue.
Traska, M. R. 1988. “Will Operating Margins Limit Access to Capital?” Hospitals 62 (2): 38–44.
United States Senate. 2023. “Letter to Commissioner Werfel and Commisioner Killen on Nonprofit Hospitals,” August 7, 2023. https://www.warren.senate.gov/imo/media/doc/Letters%20on%20Nonprofit%20Hospitals.pdf.
US Census Bureau. 2022. “Nation’s Urban and Rural Populations Shift Following 2020 Census.” Census.Gov. December 29, 2022. https://www.census.gov/newsroom/press-releases/2022/urban-rural-populations.html.
U.S. Census Bureau. n.d. “U.S. Census Bureau QuickFacts: Randolph County, Georgia.” U.S. Census Bureau. Accessed April 8, 2024. https://www.census.gov/quickfacts/fact/table/randolphcountygeorgia/PST045223.
U.S. Commission on Civil Rights. 1965. “Equal Opportunity in Hospitals and Health Facilities: Civil Rights Policies Under the Hill-Burton Program.” CCR Special Publication- Number 2. https://www.nlm.nih.gov/exhibition/forallthepeople/img/1706.pdf.
Vistnes, Gregory. 2011. “An Economic Analysis of the Certificate of Public Advantage (COPA) Agreement Between the State of North Carolina and Mission Health.” Washington, DC: Charles River Associates. https://mountainx.com/files/copareport.pdf.
Vogel, Scott. 2023. “OP-ED: Washington Can Do Better than UPMC.” SEIU Healthcare. September 19, 2023. https://seiuhcpa.org/op-ed-washington-can-do-better-than-upmc/.
Webber, David. 2018. The Rise of the Working-Class Shareholder. Cambridge, MA: Harvard University Press. https://www.hup.harvard.edu/books/9780674972131.
Weil, Jonathan. 2024. “The Private-Equity Deal That Flattened a Hospital Chain and Its Landlord.” The Wall Street Journal, May 7, 2024, sec. Markets. https://www.wsj.com/finance/the-private-equity-deal-that-flattened-a-hospital-chain-and-its-landlord-3096747d.
Wenner, David. 2023. “Closing at UPMC Hospital in Central Pa. Surprises, Worries Mayor of Rural Town – Pennlive.Com.” PennLive, January 20, 2023. https://www.pennlive.com/news/2023/01/closing-at-upmc-hospital-in-central-pa-surprises-worries-mayor-of-rural-town.html.
“WHS and UPMC Affiliation.” 2023. Washington Health System. June 20, 2023. https://whs.org/news/whs-and-upmc-affiliation/.
Wiggan, Jamie. 2023. “Pittsburgh Prepares Tax Exemption Challenges against UPMC, AHN, Other Nonprofits.” Pittsburgh City Paper, March 28, 2023. https://www.pghcitypaper.com/news/pittsburgh-prepares-tax-exemption-challenges-against-upmc-ahn-other-nonprofits-23589014.
Williams, Dunc, Kristin L. Reiter, George H. Pink, G. Mark Holmes, and Paula H. Song. 2020. “Rural Hospital Mergers Increased Between 2005 and 2016—What Did Those Hospitals Look Like?” INQUIRY: The Journal of Health Care Organization, Provision, and Financing 57 (January):0046958020935666. https://doi.org/10.1177/0046958020935666.
Wizner, Taylor. 2023. “Racism Was the Primary Reason Ohio Neighborhoods Were Redlined, New Study Shows.” Ideastream Public Media, February 3, 2023, sec. Health. https://www.ideastream.org/health/2023-02-02/racism-was-the-primary-reason-ohio-neighborhoods-were-redlined-new-study-shows.
WTAE-TV Pittsburgh, dir. 2010. Federal Gov. Investigates Braddock Hospital Closure. https://www.youtube.com/watch?v=3NLC8y9SAkY.
Young, Gary J., Chia-Hung Chou, Jeffrey Alexander, Shoou-Yih Daniel Lee, and Raver Eli. 2013. “Provision of Community Benefits by Tax-Exempt U.S. Hospitals.” New England Journal of Medicine 368 (16): 1519–27. https://doi.org/10.1056/NEJMsa1210239.
Yousufuddin, Mohammed, Maryam Mahmood, Ebrahim Barkoudah, Fatimazahra Badr, Kanika Khandelwal, Warren Manyara, Umesh Sharma, et al. 2024. “Rural-Urban Differences in Long-Term Mortality and Readmission Following COVID-19 Hospitalization, 2020 to 2023.” Open Forum Infectious Diseases, April, ofae197. https://doi.org/10.1093/ofid/ofae197.
Zanowic, Casey. 2023. “UPMC Lock Haven Is Downsizing to an Outpatient Emergency Department, the First in Pa.” WPSU, February 27, 2023. https://radio.wpsu.org/2023-02-27/upmc-lock-haven-is-downsizing-to-an-outpatient-emergency-department-the-first-in-pa.
Zumbrun, Erin Mahn. 2017. “NRHA Endorses Reintroduction of Save Rural Hospitals Act to New Congress.” National Rural Health Association. June 20, 2017. https://www.ruralhealth.us/blogs/2017/06/nrha-endorses-reintroduction-of-save-rural-hospitals-act-to-new-congress.
| Year | Law-Regulation | Content | Implications | Sources |
|---|---|---|---|---|
| 1866 | NYC Metropolitan Board of Health | Eliminated patronage in appointment of health board members; replaced political appointees with experts in sanitary science. | Enabled passage of sanitation reforms that reduced illness and death from epidemics and highly contagious diseases. Served as a model for health boards in cities across the U.S. | Grogan 2023 |
| 1894 | Wilson-Gorman Tariff Act of 1894 | Earliest statutory reference to tax exemption for certain organizations. | Passage failed, but the exemption language in the act provided the cornerstone for tax legislation re: charitable organizations for the next century. | Arnsberger, Ludlum, Riley, & Stanton. 2008 |
| 1909 | Revenue Act of 1909 | Introduced language prohibiting private inurement. | Expanded 1894 act, with explicit language that prohibits net income that “inures to the benefit of any private stockholder or individual.” | Arnsberger et al. 2008. |
| 1913 | Revenue Act of 1913 | Established income tax system with tax exemption for certain organizations. | Established tax exemptions for charitable organizations, including hospitals. | Arnsberger et al. 2008. |
| 1917-8 | Revenue Acts of 1917, 1918 | Introduced individual income tax & estate tax deductions for charitable donations. | Increased available resources for nonprofit organizations, hospitals. | Arnsberger et al. 2008. |
| 1935 | Social Security Act Title V: Maternal & Child Health Services Block Grant | Authorized annual grants to the states for maternal and child health, services for special needs children, and child welfare services. Spending focused on rural areas, those with severe economic distress. | Continued focus on prevention, but Title V introduced grants for medical care. States were funded by formula to establish service units. Child welfare services for neglected and abused children expanded in nearly all states. | Oettinger 1960; Grogan 2023 |
| 1946 | Hospital Survey and Construction Act, known as the Hill-Burton Act | Provided matching construction grants and loans to states to build new community nonprofit short-stay hospitals and nursing homes under condition that they provide ‘reasonable volume’ of free care. | Increased supply of general hospital beds; reached 1980 goal of 4.5 hospital beds/1,000 pop. Unequal distribution of state, local government matching grants, leading to exclusion of poorest areas. Institutionalized ‘separate but equal’ health facilities. | Clark, Field, Koontz and Koontz. 1980. |
| 1950 | Revenue Act of 1950 | Established the “unrelated business income tax” (UBIT) as part of the Revenue Act of 1950. | Tax-exempt organizations were still allowed to engage in a wide range of tax-free business activities on the condition that they substantially related to their tax-exempt mission, but income from unrelated businesses was taxable. | Arnsberger et al. 2008. |
| 1956 | IRS Ruling (Rev. Rul. 56-185, 1956-1 C.B. 202) | Tax exempt hospitals must provide free or below costs care to indigent patients, to the extent they are able. | Expanded access to hospital care for poor and indigent. | Arnsberger et al. 2008. |
| 1965 | Medicare & Medicaid Act (Amend 1935 SSA) | Established taxpayer-funded health insurance for the elderly (Medicare), and those on limited income (Medicaid) on a cost-plus fee-for service basis. | Led to expansion of nonprofit nursing homes and hospitals; Funded care at higher rate in for-profit versus nonprofit providers, guaranteeing for-profits a ‘risk-free’ return on investments and higher rate of growth. | Jeurissen et al. 2021 |
| 1968 | SSA T V: Maternal & Child Health Serv Block Grant | Section 242 authorizes mortgage insurance for loans to finance acute care hospital construction projects. | Increased supply of acute care hospitals. | US Dept. Housing and Urban Development. ND. |
| 1969 | Tax Reform Act of 1969 and 1969 IRS Revenue Ruling | Federal tax overhaul for nonprofit organizations. | Redefined hospitals’ responsibility from the ‘charity standard’ of indigent care to the ‘community benefit’ standard, allowing hospitals to claim credit for a broader set of activities (community health, education; medical residents). Allowed nonprofit hospitals to engage in the tax-exempt bond market. | IRS 1969; Arnsberger et al. 2008; Fox and Schaffer 1991 |
| 1983 | Tax Equity & Fiscal Responsibility Act, 1982, amended in 1983 (part of larger Social Security Bill) | Established a prospective payment system for inpatient hospital care using the diagnosis-related group (DRG) coding system. Government ends the generous reimbursements to for-profit providers for interest and depreciation on investment in facilities, including on debt related to acquisition costs | With a flat payment, hospitals and other providers keep whatever they do not spend on patient care, but have to absorb losses if the costs of patient care exceed the DRG payment. Origins of current ‘capitated’ or ‘value-based’ payment model. Hospitals raise prices charged to commercial insurers and premiums for employer-paid and individual health insurance rise dramatically. Medicare’s administered prices give federal government more control over costs. | Kimberly, Pouvourville, & D’Aunno 2008; Henderson 2015; Starr 2017 |
| 1991 | CMS Capital Prospective Payment System | Medicare replaces the reasonable cost-based (cost +) payment methodology with a capital prospective payment system (CPPS) for hospital inpatient capital-related costs – phased in over 10 years. | This was boon to smaller or poorer hospitals, with lower costs than average, but penalized wealthier hospitals with higher building costs. | Cotterill 1992 |
| 1997 | 1997 Balanced Budget Act | Reduced real (inflation adjusted) Medicare payments to hospitals in 1998-99 and extended DRG model to all types of post-acute care. | Squeezed nursing home and hospital finances, providing incentives to seek financing from capital markets. | Bazzoli, Lindrooth, Hasnain-Wynia, and Needleman. 2004. |
| 1998 | IRS Rev. Rul. 98-15 (JV Btw NP and FP entities) | IRS allowed NP hospitals to form Limited Liability Corporations (LLCs); engage in FP activities w/o paying taxes on business income they earned. | Led to dramatic growth in nonprofit hospitals setting up for-profit subsidiaries. | ReedSmith 1998 |